Abstract
INTRODUCTION: Systemic Sclerosis is a connective tissue disorder, of which skin thickening is a classical hallmark. Depending on the extent of cutaneous involvement, the disease may be diffuse or limited. A small subset (10%) of patients with Limited Systemic Sclerosis has all systemic features except the skin involvement, causing a diagnostic dilemma as discussed below.
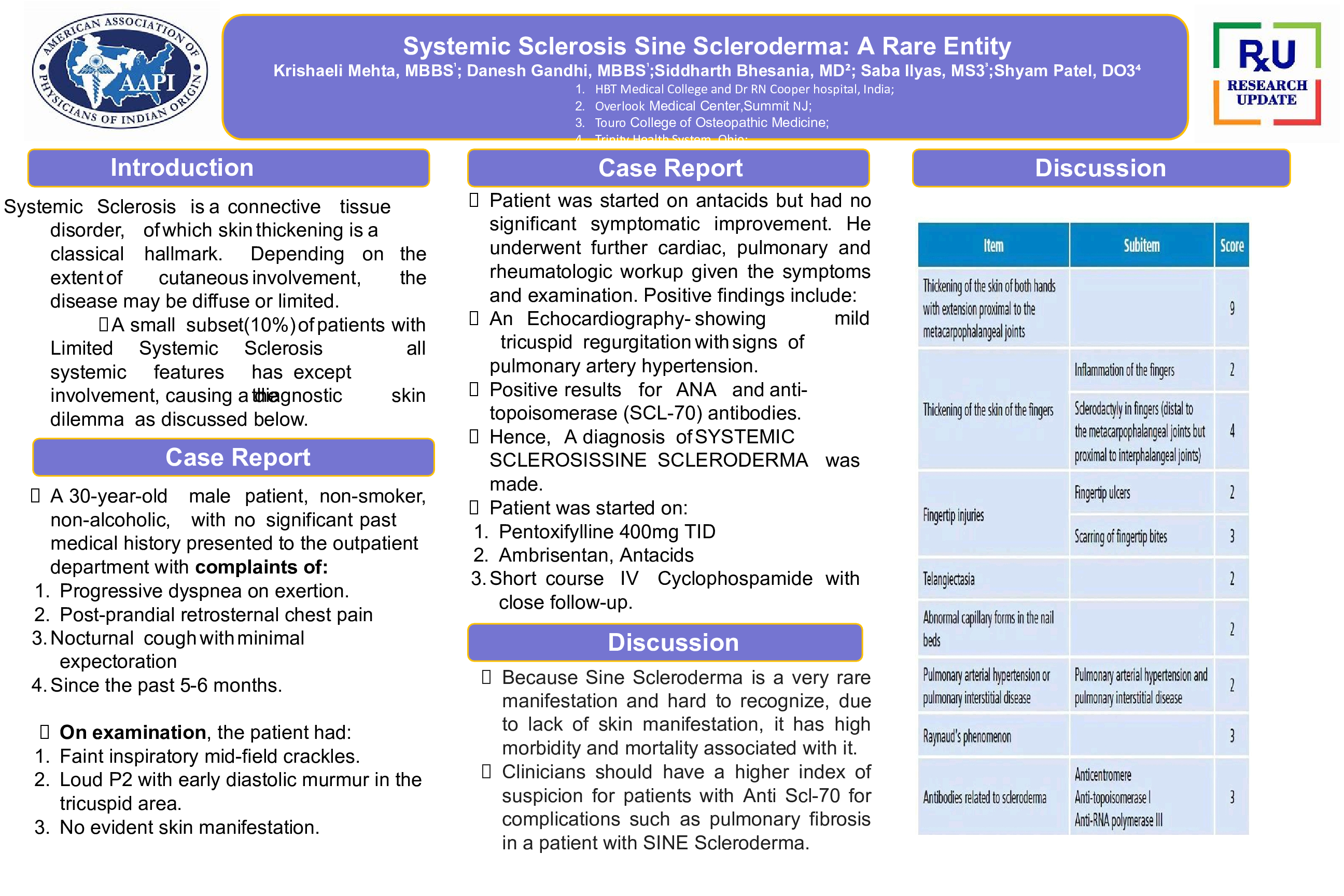
CASE: A 30-year-old male patient, non-smoker, non-alcoholic, with no significant past medical history presented to the outpatient department with complaints of: Progressive dyspnoea on exertion, Post-prandial retrosternal chest pain, Nocturnal cough with minimal expectoration since the past 5-6 months. On examination, the patient had: Faint inspiratory mid-field crackles. Loud P2 with early diastolic murmur in the tricuspid area. No evident skin manifestation. Patient was started on antacids, but had no significant symptomatic improvement. He underwent further cardiac, pulmonary and rheumatologic workup given the symptoms and examination. Positive findings include: An Echocardiography- showing mild tricuspid regurgitation with signs of pulmonary artery hypertension. Positive results for ANA and anti-topoisomerase (SCL-70) antibodies. Hence, A diagnosis of Systemic Sclerosis Sine Scleroderma was made. Patient was started on: Pentoxifylline 400mg TID. Ambrisentan, Antacids, Short course IV Cyclophospamide with close follow-up
CONCLUSION: Because Systemic Sclerosis Sine Scleroderma is a very rare manifestation and hard to recognize, due to lack of skin manifestation, it has high morbidity and mortality associated with it. Clinicians should have a higher index of suspicion for patients with Anti Scl-70 for complications such as pulmonary fibrosis in a patient with Sine Scleroderma.