Abstract
Objectives: We investigated patient characteristics and clinical outcomes of primary and secondary liver tumours treated with Stereotactic Ablative Radiotherapy (SABR) in a UK National Health Service (NHS) centre.
Methods: We undertook a retrospective analysis of patients treated with LINAC-based SABR between January 2016 and April 2019 at Guy’s Cancer Centre, London. Patient, tumor and treatment characteristics were assessed. Dose fractionations were normalized to BED10. Overall survival (OS) was evaluated using Kaplan Meier analysis and log-rank test. Only patients with a minimum follow-up of 90 days were included.
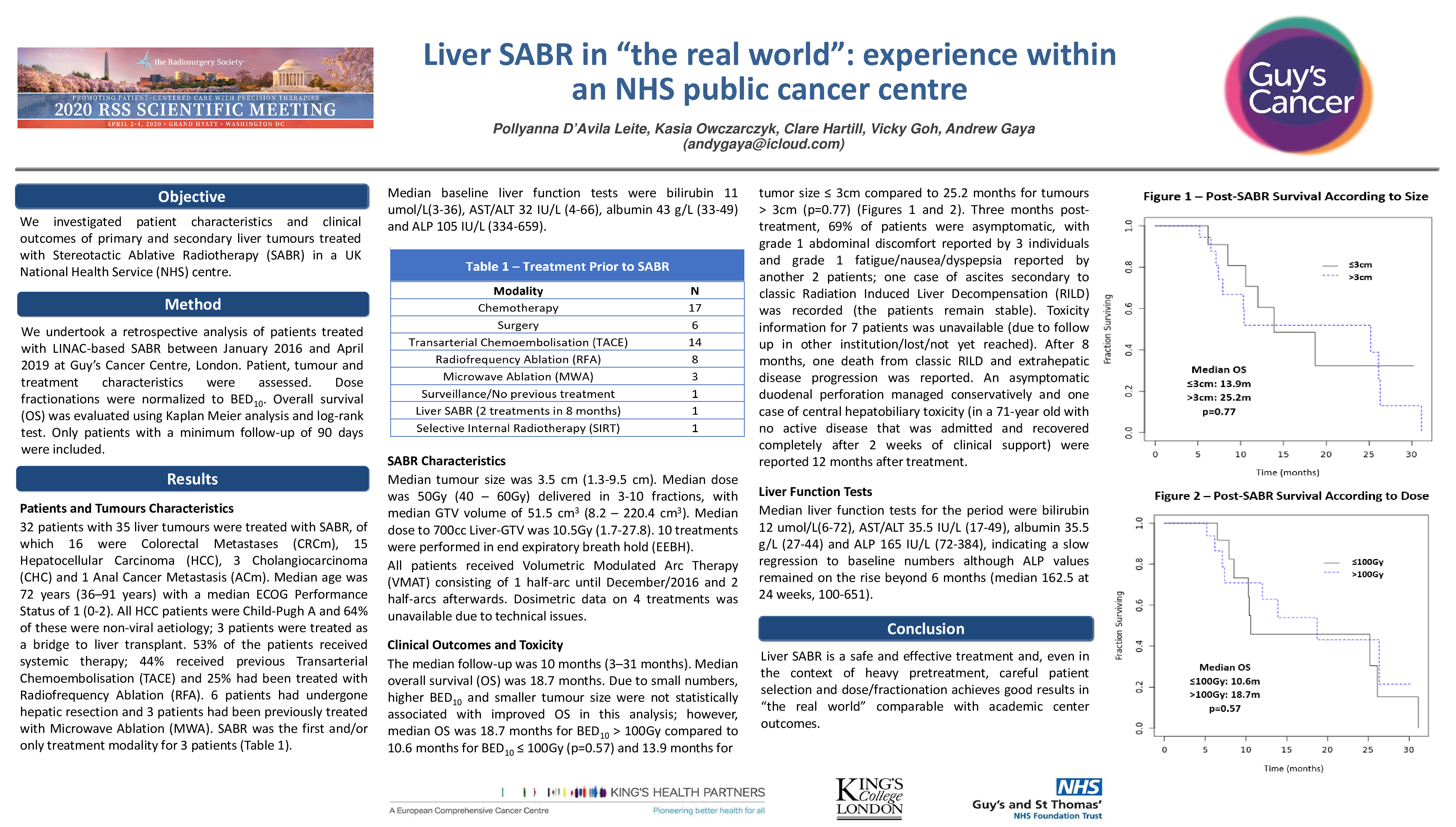
Results: 32 patients with 35 liver tumours were treated with SABR, of which 16 were Colorectal Metastases (CRCm), 15 Hepatocellular Carcinoma (HCC), 3 Cholangiocarcinoma (CHC) and 1 Anal Cancer Metastasis (ACm). Median age was 72 years (36–91 years) with a median ECOG Performance Status of 1 (0-2). All HCC patients were Child-Pugh A and 64% of these were non-viral aetiology; 3 patients were treated as a bridge to liver transplant. 53% of the patients received systemic therapy; 44% received previous Transarterial Chemoembolisation (TACE) and 25% had been treated with Radiofrequency Ablation (RFA). 6 patients had undergone hepatic resection and 3 patients had been previously treated with Microwave Ablation (MWA). SABR was the first and/or only treatment modality for 3 patients. Median baseline liver function tests were bilirubin 11 umol/L(3-36), AST/ALT 32 IU/L (4-66), albumin 43 g/L (33-49) and ALP 105 IU/L (334-659). The median follow-up was 10 months (3–31 months). Median tumor size was 3.5 cm (1.3-9.5 cm). Median dose was 50 Gy (40 – 60 Gy) delivered in 3-10 fractions, with median GTV volume of 51.5 cm3 (8.2 – 220.4 cm3). Median dose to 700cc Liver-GTV was 10.5Gy (1.7-27.8). 10 treatments were performed in end expiratory breath hold (EEBH). Median overall survival (OS) was 18.7 months. Due to small numbers, higher BED10 and smaller tumour size were not statistically associated with improved OS in this analysis; however, median OS was 18.7 months for BED10 > 100 Gy compared to 10.6 months for BED10 ≤ 100 Gy (p=0.57) and 13.9 months for tumor size ≤ 3cm compared to 25.2 months for tumors > 3cm (p=0.77). Three months post-treatment, 69% of patients were asymptomatic, with grade 1 abdominal discomfort reported by 3 individuals and grade 1 fatigue/nausea/dyspepsia reported by another 2 patients; one case of ascites secondary to classic Radiation Induced Liver Decompensation (RILD) was recorded (the patients remains stable). Median liver function tests for the period were bilirubin 12 umol/L(6-72), AST/ALT 35.5 IU/L (17-49), albumin 35.5 g/L (27-44) and ALP 165 IU/L (72-384), indicating a slow regression to baseline numbers although ALP values remained on the rise beyond 6 months (median 162.5 at 24 weeks, 100-651). After 8 months, one death from classic RILD and extrahepatic disease progression was reported. An asymptomatic duodenal perforation managed conservatively and one case of central hepatobiliary toxicity were reported 12 months after treatment.
Conclusions: Liver SABR is a safe and effective treatment and, even in the context of heavy pretreatment, careful patient selection and dose/fractionation achieves good results in “the real world” comparable with academic center outcomes.