Abstract
Objective(s)
In an integrated MR-guided brachytherapy (MRgBT) suite, the patient remains in one location and a MR system mounted on ceiling rails move in and out of the interventional suite as needed. General anesthesia (GA), applicator insertion, MR-image acquisition and high-dose-rate (HDR) BT delivery can take place in the same room. Real-time MR-image acquisition has the potential to substantially improve overall procedure efficiency and interstitial needle placement (hence improve target coverage and dose sparing to organs at risk). The aim of this work is to describe our experience in implementing our first real-time MR-guided interstitial BT treatment for a gynecological (GYN) patient.
Methods
Process mapping defining tasks and workflow was completed and checklists development was done. Safety policies/procedures regarding radiation and MR safety for staff and patients were established. Interdisciplinary team meetings and structured walk-throughs with anesthesiologists, anesthesia assistants, radiation oncologists, nurses, MR technologists and brachytherapists were held to design a safe procedure. Equipment flow and room transition were proposed: surgical, MR and radiation safety checks were incorporated in the intra-op MR-guided BT procedure. Lastly, mock emergency scenarios were discussed prior to scheduling the first patient.
Results
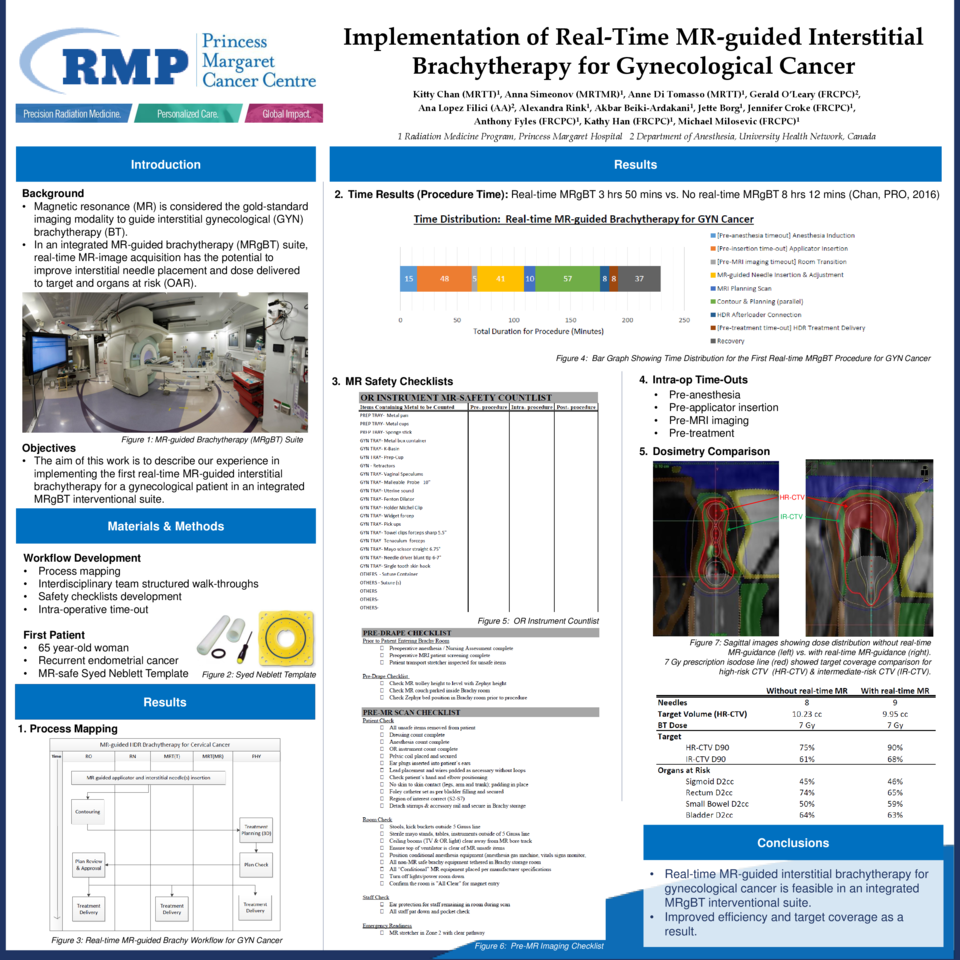
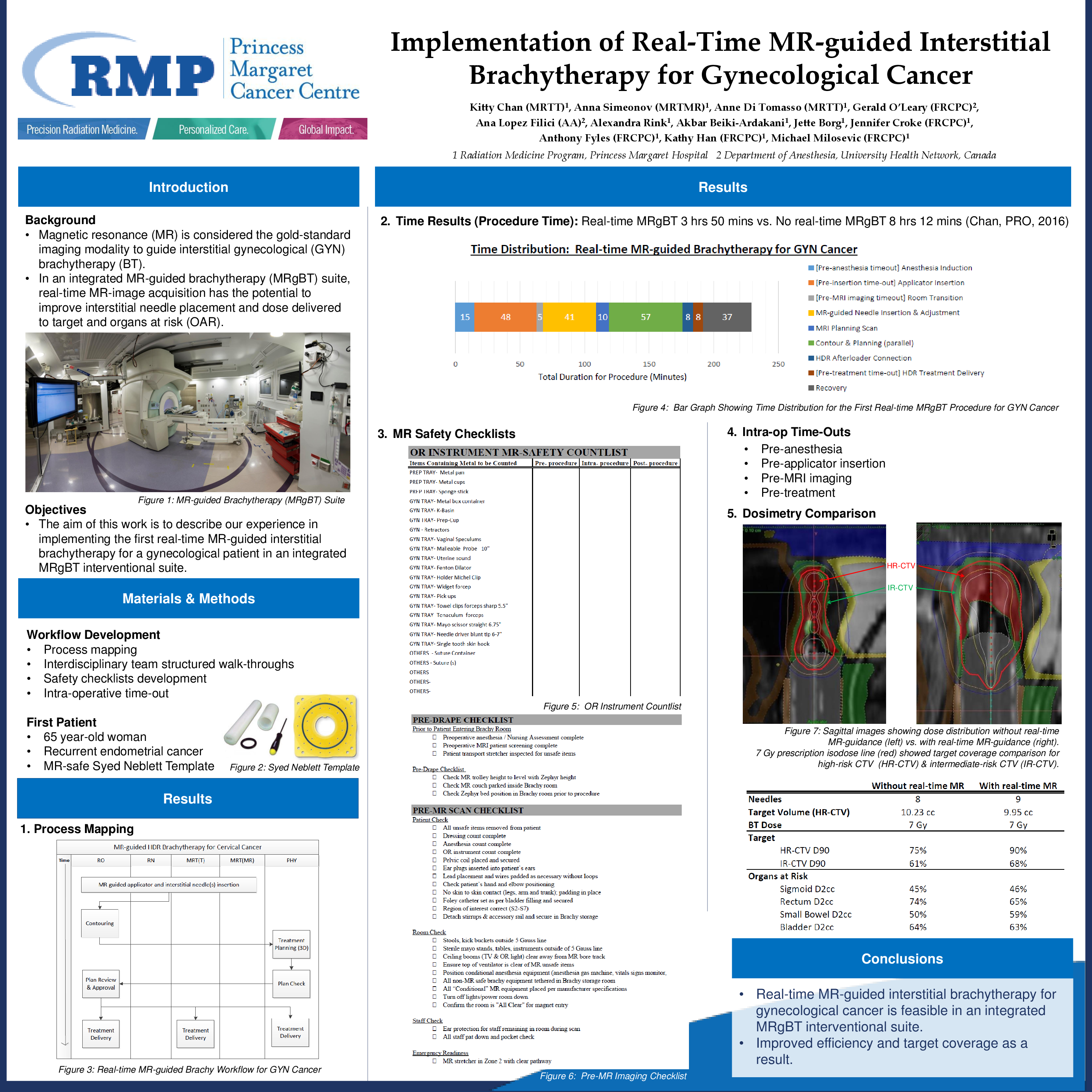
Four safety time-outs were executed: pre-anesthesia, pre-applicator insertion, pre-MRI imaging & pre-HDR treatment. Four checklists: pre-drape & pre-MR scan, one surgical instrument and one anesthesia equipment/supplies checklists were developed to ensure surgical and MR safety. A 65 year-old woman with vaginal recurrence of endometrial cancer underwent real-time MR-guided interstitial BT using Syed-Neblett template under GA in the MRgBT suite. Total procedure time was 3 hours and 13 min (from GA induction to completion of HDR BT delivery): applicator and template insertion (48 mins), MR-guided needle insertion (41 mins), contouring and planning (30 mins), HDR BT delivery (8 mins) and recovery (37 mins). Time savings of 65% was achieved compared with procedure performed in a non-integrated MRgBT suite setting (9 hrs 6 mins). For a 7 Gy prescription, dosimetry improved from first insertion (without real-time MR) to second insertion (with real-time MR): the D90% ,V100 for CTVHR & CTVIR : 7.7 to 12.6Gy, 83% to 99% & 4.1 to 6.7Gy, 91% to 100%. Changes to D2cc for Sigmoid, Rectum, Small Bowel & Bladder were as follows: 0.47 to 1.12Gy, 4.9 to 3.6Gy, 1.7 to 3.6Gy & 3.8 to 3.58Gy. The EQD2 dose combining external beam radiotherapy 45 Gy (1.8 Gy/fraction) and two HDR BT for CTVHR & CTVIR, Sigmoid, Rectum, Small Bowel & Bladder were: 90 Gy, 68 Gy, 46 Gy, 65 Gy, 59 Gy & 63 Gy.
Conclusions
Our initial experience demonstrates that real-time MR-guided interstitial BT treatment for GYN cancer is feasible in an integrated MRgBT interventional suite; substantial efficiency and target coverage were improved as a result.