Abstract
BACKGROUND: Therapeutic inertia and lack of compliance are the main
barriers to hypertension control
OBJECTIVES: Presentation of a case illustrating the importance of
proper adherence to blood pressure and a detailed anamnesis in
patients with apparent refractory hypertension.
METHODS: Review of the clinical record.
RESULTS: A female patient had been diagnosed of hypertension 3 years
ago, with SBP around 150-160 mmHg and DBP around 90-100 mmHg.
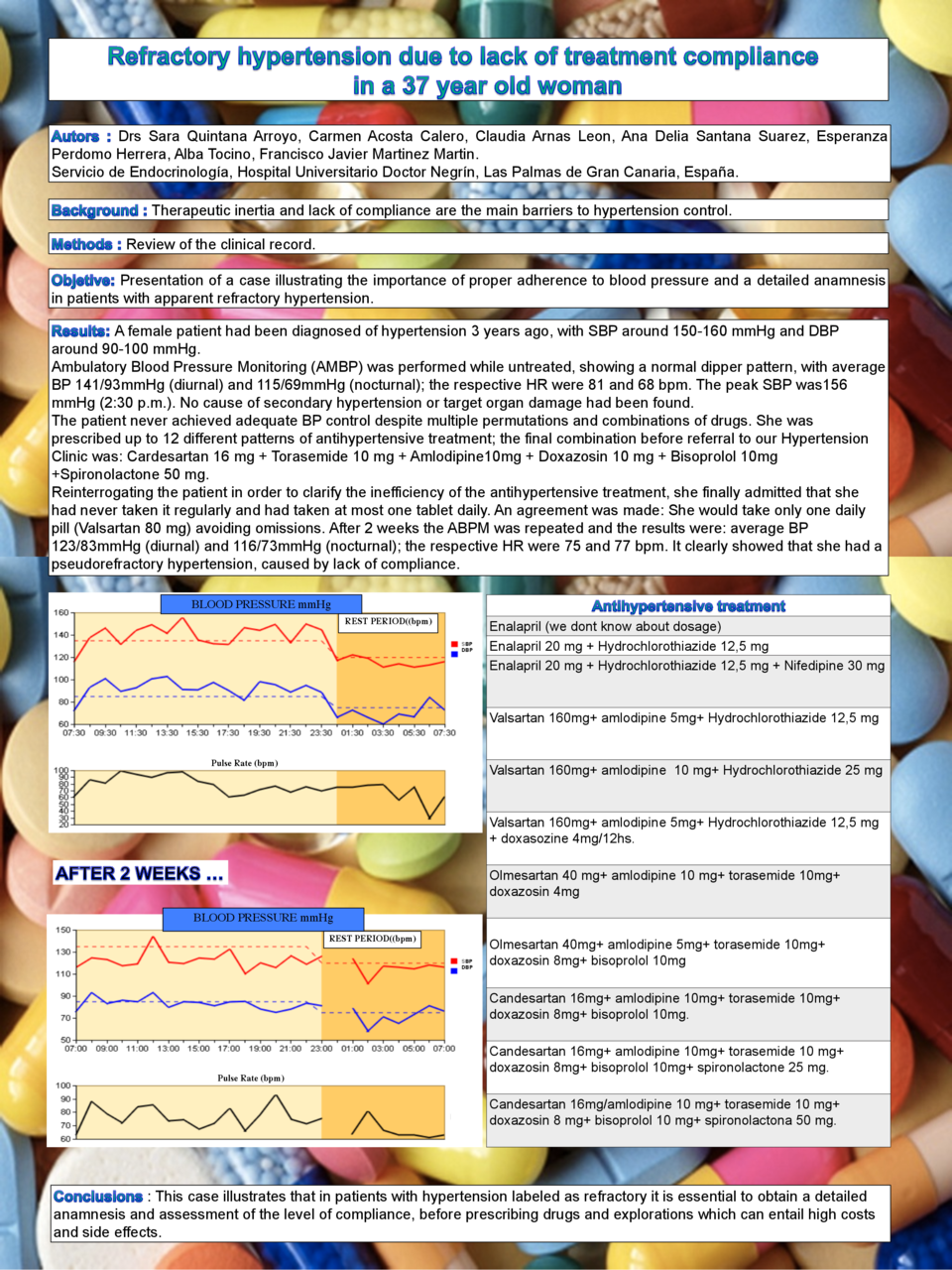
Ambulatory Blood Pressure Monitoring (AMBP) was performed while
untreated, showing a normal dipper pattern, with average BP 141/93mmHg
(diurnal) and 115/69mmHg (nocturnal); the respective HR were 81 and 68
bpm. The peak SBP was156 mmHg (2:30 p.m.). No cause of secondary
hypertension or target organ damage had been found.
The patient never achieved adequate BP control despite multiple
permutations and combinations of drugs. She was prescribed up to 12
different patterns of antihypertensive treatment; the final
combination before referral to our Hypertension Clinic was:
Cardesartan 16 mg + Torasemide 10 mg + Amlodipine10mg + Doxazosin 10
mg + Bisoprolol 10mg +Spironolactone 50 mg. Reinterrogating the
patient in order to clarify the inefficiency of the antihypertensive
treatment, she finally admitted that she had never taken it regularly
and had taken at most one tablet daily. An agrrement was made: She
would take only one daily pill (Valsartan 80 mg) avoiding omissions.
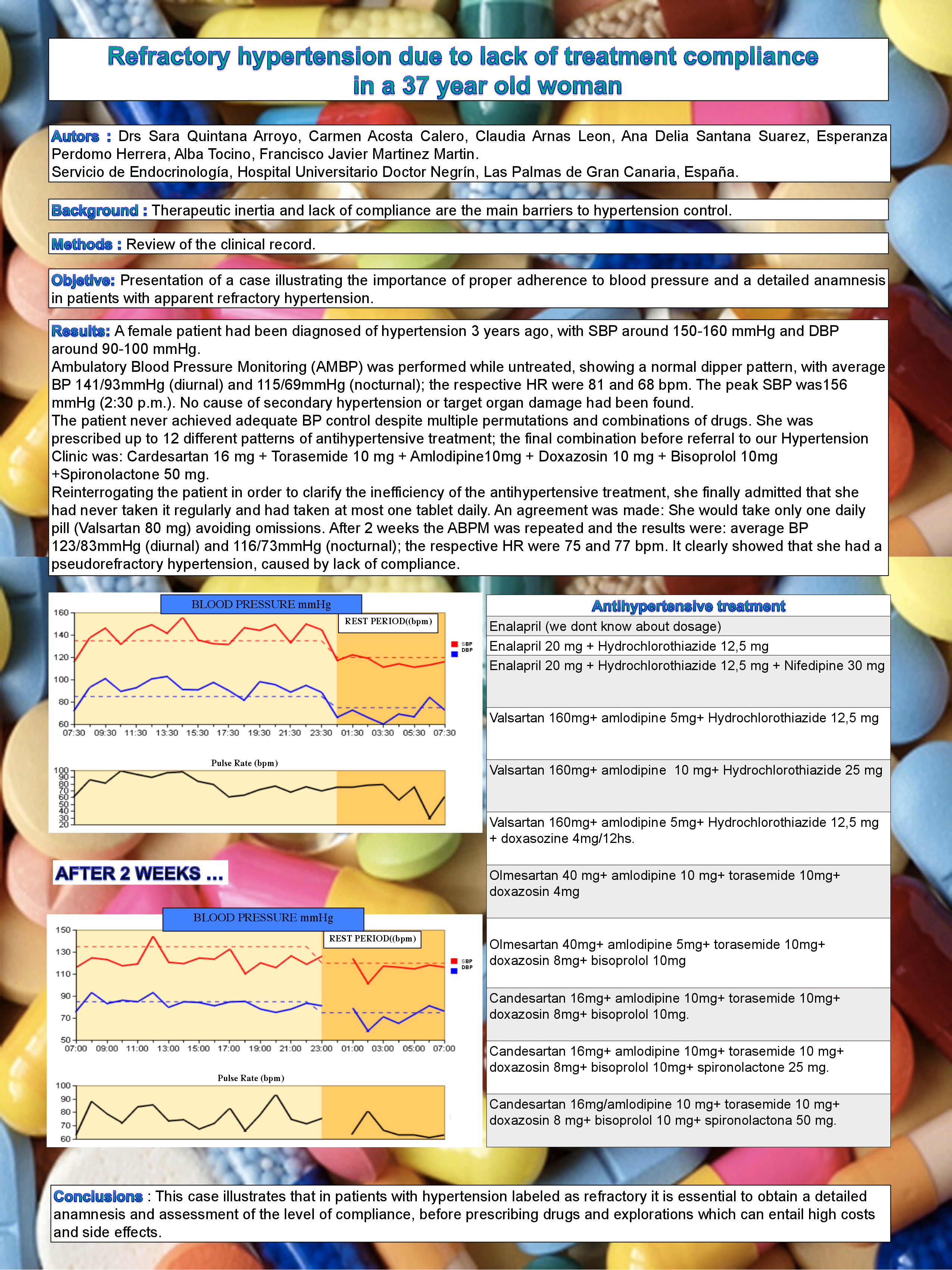
After 2 weeks the ABPM was repeated and the results were: average BP
123/83mmHg (diurnal) and 116/73mmHg (nocturnal); the respective HR
were 75 and 77 bpm. It clearly showed that she had a pseudorefractory
hypertension, caused by lack of compliance.
CONCLUSIONS: This case illustrates that in patients with hypertension
labeled as refractory it is essential to obtain a detailed anamnesis
and assessment of the level of compliance, before prescribing drugs
and explorations which can entail high costs and side effects.