Abstract
Purpose: A wide variation of the rate of radiotherapy (RT) received by patients in Ontario exists depending on hospital of cancer diagnosis, more than explained by studied factors affecting RT use such as on-site RT, distance from RT centre, patient age, and income. To reach patients in hospitals without on-site RT, Ontario cancer centres have employed outreach activities. There is no current provincial policy on Radiation Oncology (RO) outreach and the extent of outreach is unknown. Our purpose was to describe and compare all RO outreach activities by Ontario cancer centres.
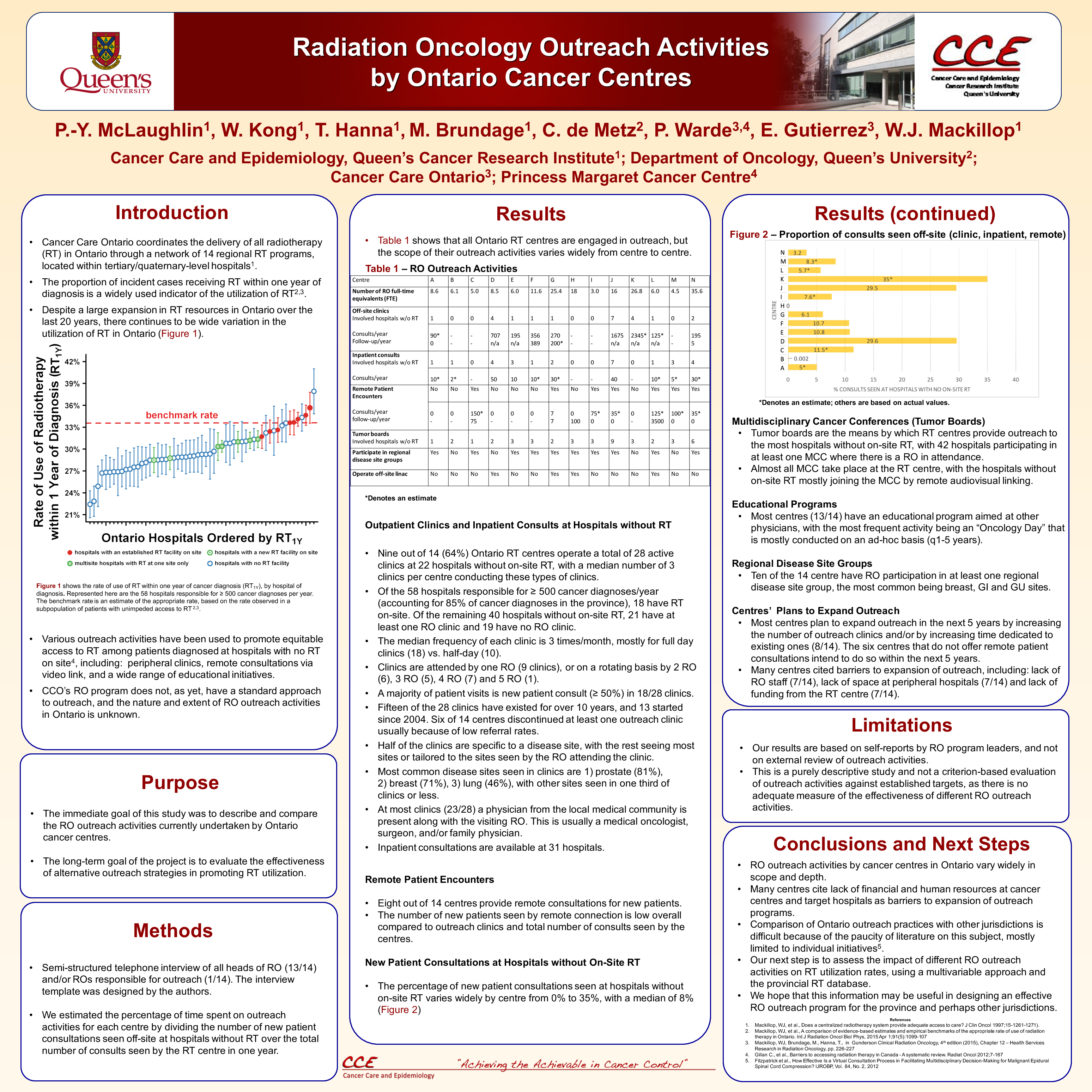
Materials and Methods: We conducted a semi-structured interview of leaders of all 14 of the Ontario cancer centres.
Results: Heads of 14/14 Ontario cancer centres responded and completed the interview. No centres declined interview. Nine of 14 centres have at least one outreach clinic in hospitals without on-site RT for a total of 28 clinics in 22 involved hospitals without on-site RT. Disease sites most often seen are prostate, breast, lung and least commonly pediatric, head and neck and sarcoma. Clinic frequency varies greatly, occurring at a median frequency of 3 days/month (range: once/2 months to 2 days/week). Twenty-three out of 28 clinics have another physician present in the same clinic the most common: medical oncologist, surgeon, and family doctors. Inpatient consultations are provided in 31 hospitals without on-site RT, all most all for palliative indications (90%), with most having this service take place concurrently with the outpatient clinics. Eight out of 14 centres provide remote patient encounters, with low numbers of consults (4-125 patients/year) and total number of patients except for one centre which has at least 3500 encounters/year, and all mostly for follow-ups (90%). All centres have multidisciplinary cancer conferences involving hospitals without on-site RT, mostly by virtual linking (13/14). Most centres (10/14) participate in regional disease site groups, the most common being breast, GU and GI with others much less frequently. Most centres participate in educational outreach aimed at off-site physicians. All centres plan to expand outreach activities, most commonly with more outreach clinics (8/14) and starting remote patient encounters (6/14). Most cited barriers to more RO outreach are lack of funding from own centre for outreach, lack of funding at peripheral hospital and lack of available RO staff.
Conclusions: RO outreach activities by Ontario cancer centres have a highly variable scope depending on the centre and have overall low uptake, explained by lack of financial and human resources. All centres intend to expand outreach activities within the next 5 years. Our next step is to correlate of outreach status of individual Ontario hospitals without on-site RT with RT use, using the provincial RT database and a multivariable approach.