Abstract
Background: Prostate cancer (PCa) affects one in six men, and of these, for one in six it will be fatal. Most cases are indolent, yet for many it is aggressive and metastasizes to bone, lymph nodes or to soft tissue organs. PCa has many similarities with breast cancer, and with only a slightly lower mortality rate.
Aim & Objectives: Many new therapies have been developed in recent years for advanced PCa, and far more are under development. The objective is to review these developments (proven and unproven) and to assess the practical impact they have on patients. The author is both a scientist and the patient.
Methods/Study Design: A review of recent literature was conducted to evaluate the potential of approved therapies (in the USA) on advanced prostate cancer. A historical search was made of earlier developments as well to determine how they have influenced current thinking and advances.
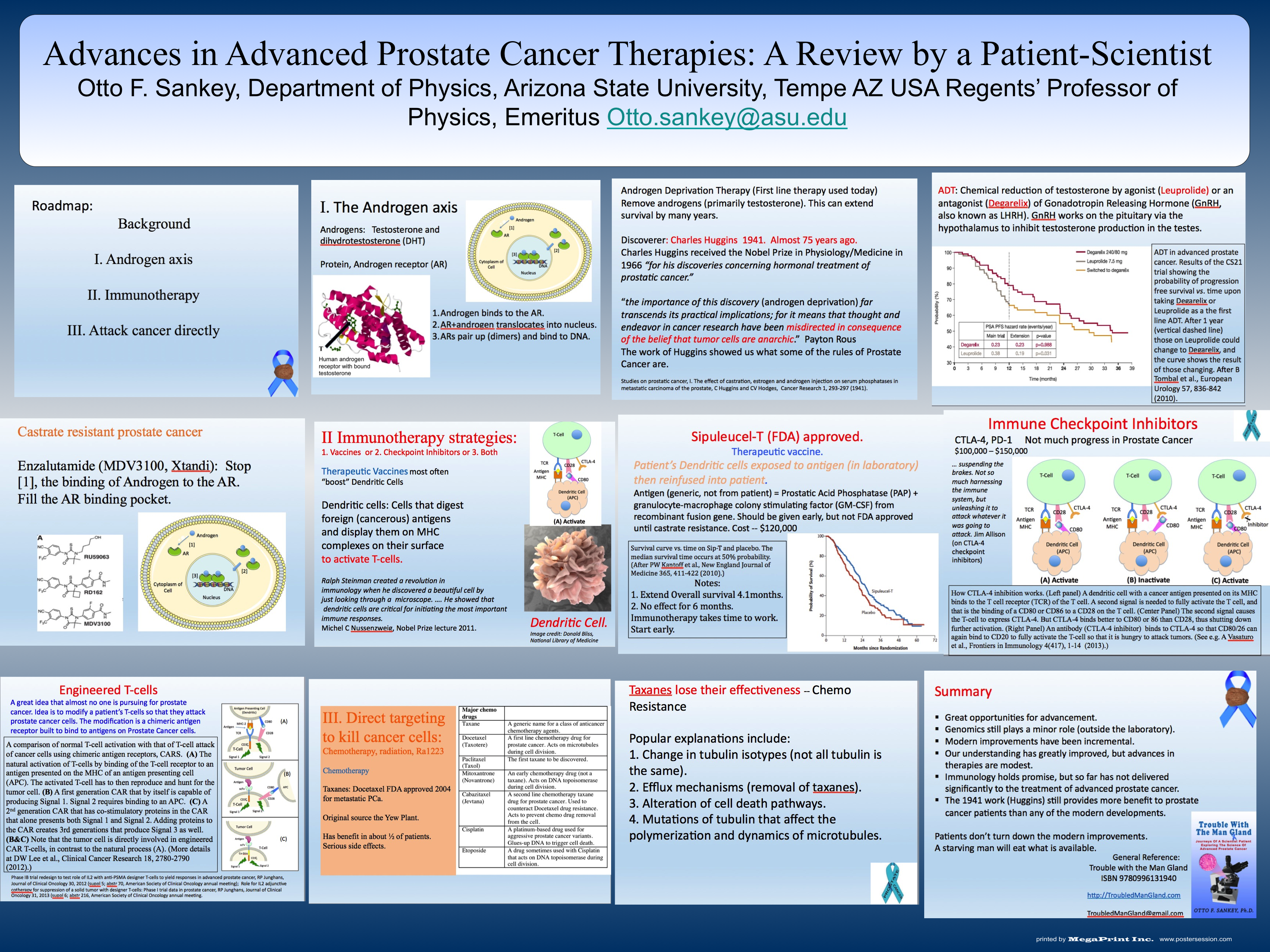
Results/Findings: There are at least three major therapy classifications for advanced PCa.
They are (1) Interference within the androgen axis, (2) attacking cancer by using, or modifying, the patient’s immune system (immunotherapy), and (3) killing the cancer directly by chemo-therapeutic drugs, or targeted drugs.
(1) The androgen axis focuses on disabling the androgen receptor (AR) from translocating the nuclear membrane and activating genes within DNA for growth and reproduction of PCa cells. Androgens (testosterone, DHT) activates the AR by binding in a pocket within the AR. Strategies for interfering with the androgen axis include inhibiting androgen production (GnRH agonist or antagonists, castration), altering the pathway of cholesterol to androgen transformation by enzyme inhibition (Abiraterone Acetate, AA), inhibiting the binding of androgen (Enzalutamide, ENZ), or inhibiting the binding of the AR with DNA (Bromodomain inhibitor, experimental JQ1).
(2) The immune system is used to attack PCa cells with therapeutic vaccines generally by modifying dendritic cells (DCs). The Sipuleucel-T (ST) therapy exposes patient’s DCs to non-patient PAP antigens. Other variations include engineered viruses that express prostate cancer related antigens like PSA (Prostvac). Attempts have also been made to use checkpoint inhibitors CTLA-4 and PD-1, and to directly engineer T-cells.
(3) Finally there are drug therapies directed to kill cancer cells. Taxanes alter the dynamics of microtubules, which interpret cell mitosis and enhance apoptosis (Docetaxel or Cabazitaxel). Platins, especially used for neuroendocrine PCa, binds to DNA interfering with cell division.