Abstract
Alexander Louie1, Mark Mishra2, Vinai Gondi3, Minesh Mehta2
1VU University Medical Center, Amsterdam, Netherlands
2University of Maryland, Baltimore, MD
3University of Wisconsin, Madison, WI
Purpose: The standard of care for patients with limited stage small cell lung cancer (LS-SCLC) is definitive chemoradiation followed by prophylactic cranial irradiation (PCI) for patients who achieve a partial or complete response to initial therapy. PCI has been shown to increase overall survival, but at the cost of neurocognitive dysfunction. RTOG 0933 has recently demonstrated that hippocampal avoidance (HA) during whole brain radiation therapy is associated with decreased neurocognitive dysfunction, but also a small increased risk for brain metastasis (BM) within the peri-hippocampal region. The primary objective of this analysis is to determine which strategy (PCI with or without HA) results in greater quality-adjusted life expectancy (QALE) for LS-SCLC using Markov modelling. Secondary objectives are to determine: 1) what relative decrease in neurocognitive dysfunction is required to justify using PCI with HA, and 2) what is the maximum acceptable increase in risk for developing BM that can still justify HA.
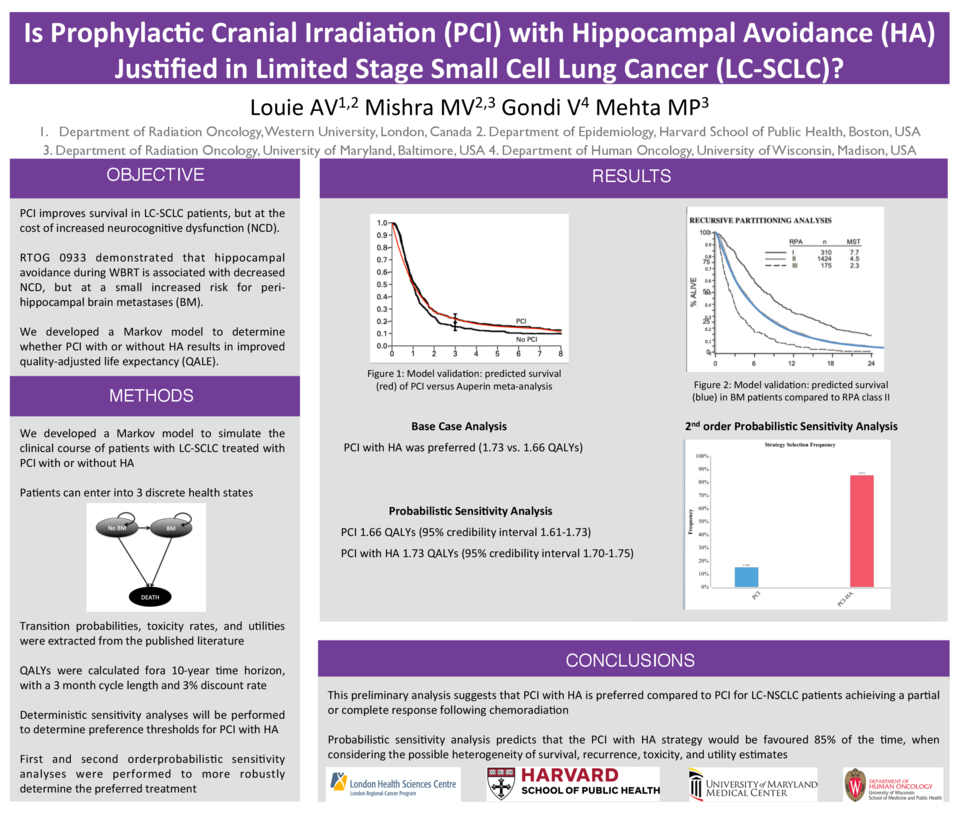
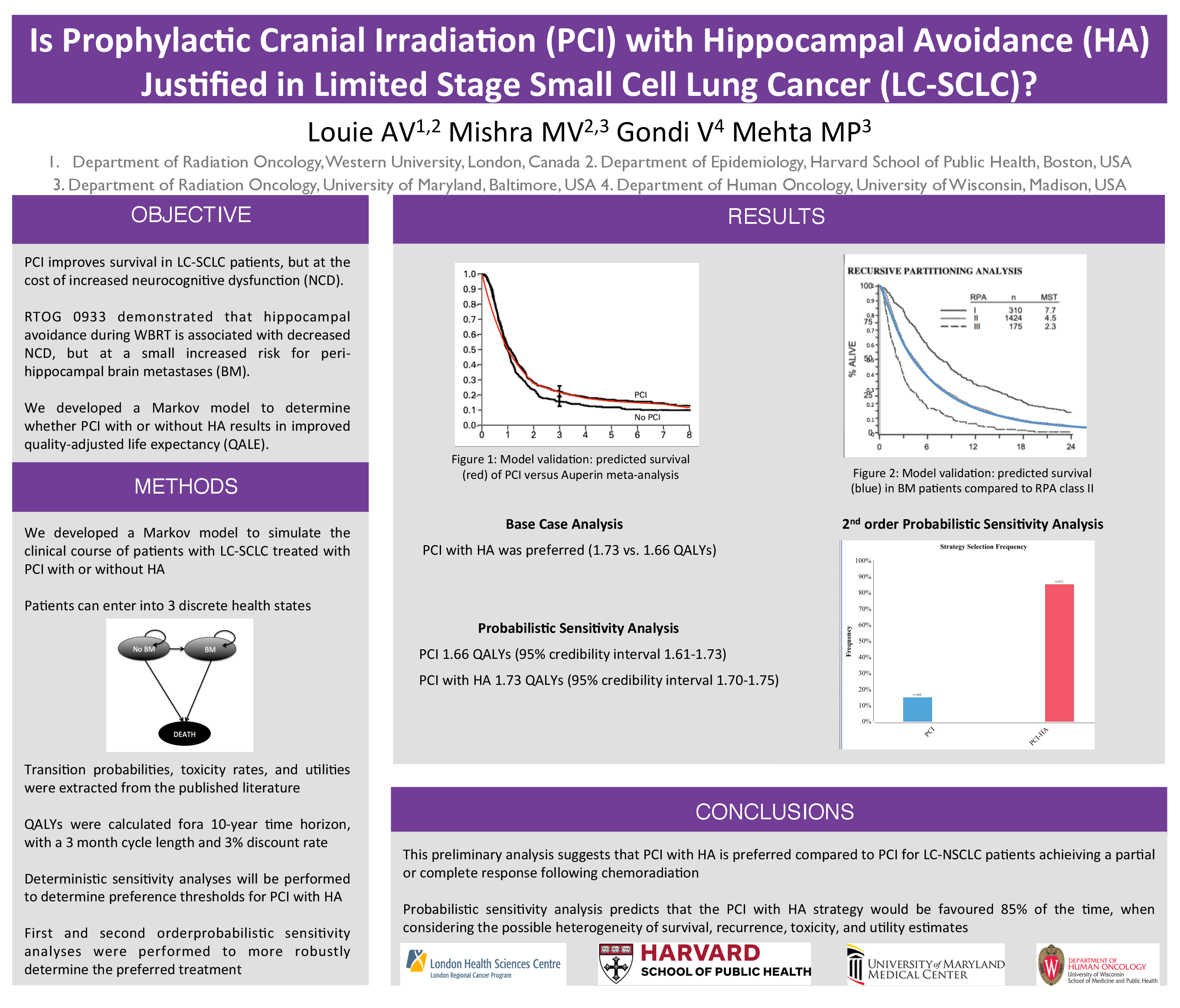
Materials and Methods: We developed a Markov model to simulate the clinical course of a cohort of patients with LS-SCLC, receiving PCI with or without HA. The following health states were incorporated into the Markov model: 1) Well (no evidence of disease, and no neurocognitive dysfunction); 2) Neurocognitive Dysfunction (no evidence of disease, but neurocognitive dysfunction); 3) Cranial Disease (development of BM); 4) Cranial Disease and Neurocognitive Dysfunction (BM and neurocognitive dysfunction); and 5) Dead. Utility values for each Markov state, and transition probabilities between Markov states, were extracted from the published literature. The model was internally validated to demonstrate overall survival outcomes closely correlated to the source data. One- and two-way sensitivity analyses were performed to determine the thresholds at which PCI with HA would be preferred. A 10-year time horizon using a cycle length of three months was employed and quality adjusted life years (QALYs) were discounted at a rate of 3%.
Results: The results of this analysis demonstrate that in the reference scenario, PCI with HA is associated with improved QALE (3.56 versus 3.49 QALYs). Sensitivity analyses demonstrate that PCI with HA is the preferred treatment approach provided that the risk of developing brain metastases is not increased by >11.9%. HA with PCI is also the preferred treatment approach provided that rates of neurocognitive dysfunction are reduced by at least 21.4% compared to PCI without HA.
Conclusions: This model suggests that PCI with HA is associated with improved QALE. Results of the present study can inform the statistical design of a future Phase III study examining the relative merits of PCI with or without HA.