Abstract
Introduction: Lysergic acid diethylamide (LSD) is part of the pharmacological group known as “classical hallucinogens” or “psychedelics” (term coined by Humphrey Osmond in 1957). LSD, taken at moderate doses, produces changes in body perception, time distortion, and psychotropic effects, often described as “mystical experiences.” While LSD is currently a Schedule 1 drug and not FDA-approved, research has shown that LSD-assisted psychotherapy may positively impact patients suffering from illness-related anxiety, depression, psychosomatic conditions, substance abuse, and cancer-induced pain disorders. However, these hallucinogens carry some risk, one of them includes a dangerous state of anxiety and psychosis, causing unpredictable behaviors in an uncontrolled environment. We present a case highlighting the importance of identifying the adverse side effects of LSD and its risk of lowering one’s threshold for developing schizophrenia.
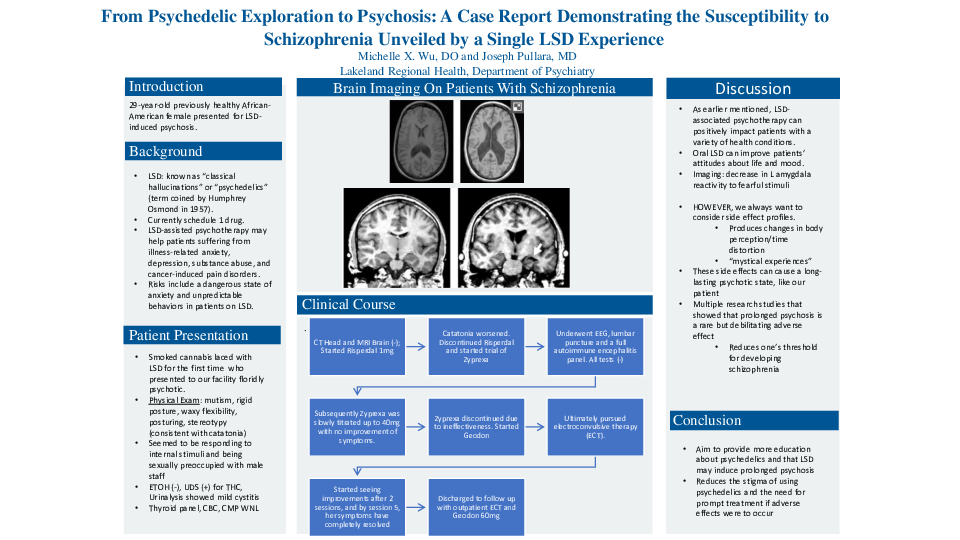
Case Description: This is a case of a 29-year-old previously healthy African American female with no known family history of psychosis, who apparently smoked cannabis laced with LSD, presented to our facility a few days later floridly psychotic and as family stated “unrecognizable.” On initial evaluation, she was AAO x 0 and appeared paranoid about her surroundings. She seemed to be responding to internal stimuli while mumbling repetitive phrases such as “Whiskey Mike” and “imposter syndrome” without further elaboration. On physical examination, she was exhibiting catatonic symptoms such as mutism, rigid posture, waxy flexibility, posturing, agitation, and stereotypy. Due to the abrupt onset of symptomatology, our initial goal was to rule out any organic causes or conditions of autoimmune origin. CT head, MRI brain, EEG, lumbar puncture, and a full autoimmune panel were all negative. Throughout the course of her hospitalization, it became clearer that her psychosis was worsening. She demonstrated increasingly self-destructive behaviors such as banging her head on furniture and scratching herself. Additionally, she was physically aggressive to her peers and became sexually preoccupied by male peers and staff. She failed multiple antipsychotics such as risperidone and olanzapine; however, ziprasidone showed slight improvements. Ultimately, we decided to pursue electroconvulsive therapy (ECT) which showed drastic improvements. After merely 5 treatments, her symptoms had completely resolved, and she was discharged to follow up with outpatient ECT treatments.
Discussion: With the increasing research on psychedelics for the treatment of psychiatric conditions, it is also important to note the potential side effects of these substances. This case adds to the growing literature related to LSD-induced psychosis and catatonia with a previously healthy patient without a known family history of psychotic disorders. Previous research from Breakey et al. conducted a comprehensive history of 46 schizophrenic patients with 46 matched controls and discovered that schizophrenics who had used hallucinogens experienced onset of psychosis on average four years earlier than non-users. Our goal is to educate providers on the importance of early treatments to provide patients with better prognosis and quality of life.