Abstract
Introduction: In 2018, the prevalence of sexually transmitted infections (STIs) in the United States (U.S.) was estimated to be 67.6 million, which accounts for approximately 20% of the U.S. population1. Additionally, individuals aged 15-24 comprised 45.5% of all incident infections in 20181. 93.1% of all incident infections in 2018 can be attributed to chlamydia, trichomoniasis, genital herpes, and human papillomavirus (HPV)1. Incident STIs in 2018 imposed an estimated $15.9 billion burden in lifetime medical costs2. During 2017-2019, in data from 45 jurisdictions, 76.2% of women aged 18-49 were considered at-risk for unintended pregnancy3. Unintended pregnancies account for nearly 50% of all U.S. pregnancies and are associated with both maternal and infant adverse health outcomes3. STIs and unintended pregnancies are continuous public health concerns, and this study aims to identify discrepancies in contraceptive method use in relation to demographics that include age, race, education, marital status, and insurance status.
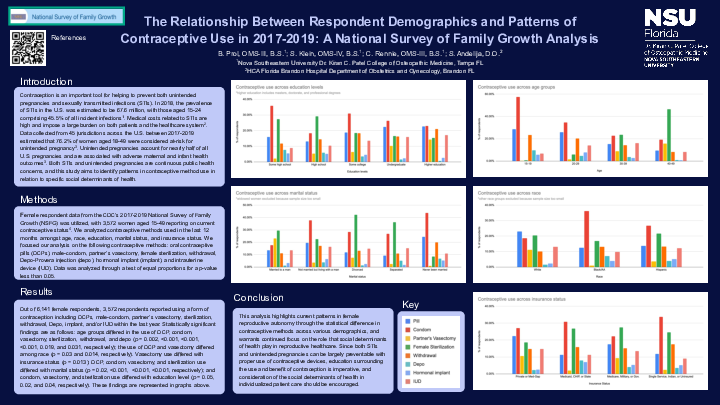
Methods: We utilized female respondent data of 6,141 women aged 15-49 from the CDC’s 2017-2019 National Survey of Family Growth (NSFG) report on current contraceptive status. We analyzed contraceptive methods used in the last 12 months amongst age, race, education, marital status, and insurance status. We analyzed the following contraceptive methods: oral contraceptive pills (OCPs), male-condom, partner’s vasectomy, female sterilization, withdrawal, Depo-Provera injection (depo), hormonal implant (implant), and intrauterine device (IUD). Data was analyzed through a test of equal proportions for p-value less than 0.05.
Results: Out of 6,141 total female respondents, 3,572 respondents reported using OCPs, male-condom, partner’s vasectomy, sterilization, withdrawal, Depo, implant, and/or IUD within the last year. Age groups differed in the use of OCP, condom, vasectomy, sterilization, withdrawal, and depo (P=.002, <.001, <.001, <.001, .02, and .03, respectively). The use of OCP and vasectomy differed among race (P=.03 and .01, respectively). Condom, vasectomy, and sterilization use differed with education level (P=.05, .02, and .04, respectively). OCP, condom, vasectomy, and sterilization use differed with marital status (P=.02, <.001, <.001, <.001, respectively). Vasectomy use differed with insurance status (P=.01).
Conclusion: This analysis highlights gaps that are present in female reproductive autonomy through the statistical difference in contraceptive methods across various demographics, and warrants continued focus on the role that social determinants of health play in the prevention of unintended pregnancies and STIs.