Abstract
Introduction: Primary sclerosing cholangitis (PSC) is a rare condition affecting an estimated 1 in 10,000 people and has a diagnosis rate of 1 in 100,000 people per year. PSC is believed to be an autoimmune disease that is generally detected in 30- to 40-year-old male patients, which occurs due to patients' immune cells attacking the intra- and extrahepatic bile ducts leading to inflammation that leads to scarring and ultimately blockage of bile excretion. This bile buildup can lead to liver cirrhosis and even failure. Signs and symptoms of PSC include fatigue, weight loss, abdominal discomfort, pruritus, jaundice, and splenomegaly. Seventy percent of patients with PSC often have a comorbid condition called Inflammatory bowel disease (IBD), with Ulcerative Colitis (UC) being the most common form. PSC patients are at an elevated risk of developing cancers of the gallbladder, bile ducts, colon, and liver. Unfortunately, there are currently no FDA approved treatments to stop the progression of PSC. A liver transplant may prolong life in patients who progress to liver failure but is not always curative.
Case Description: We present the case of a 48-year-old Caucasian male patient who initially presented to the ER with fever of 103.4°F, tachycardia, headache, dizziness, chills, right sided abdominal pain with radiation to his back, and fatigue for the past 3 days with weight loss of more than 20 lbs. over the past month. The patient has a medical history of Primary Sclerosing Cholangitis (PSC) diagnosed in 2020, Ulcerative Colitis (UC) diagnosed in 2019, and stage 3 liver cirrhosis.
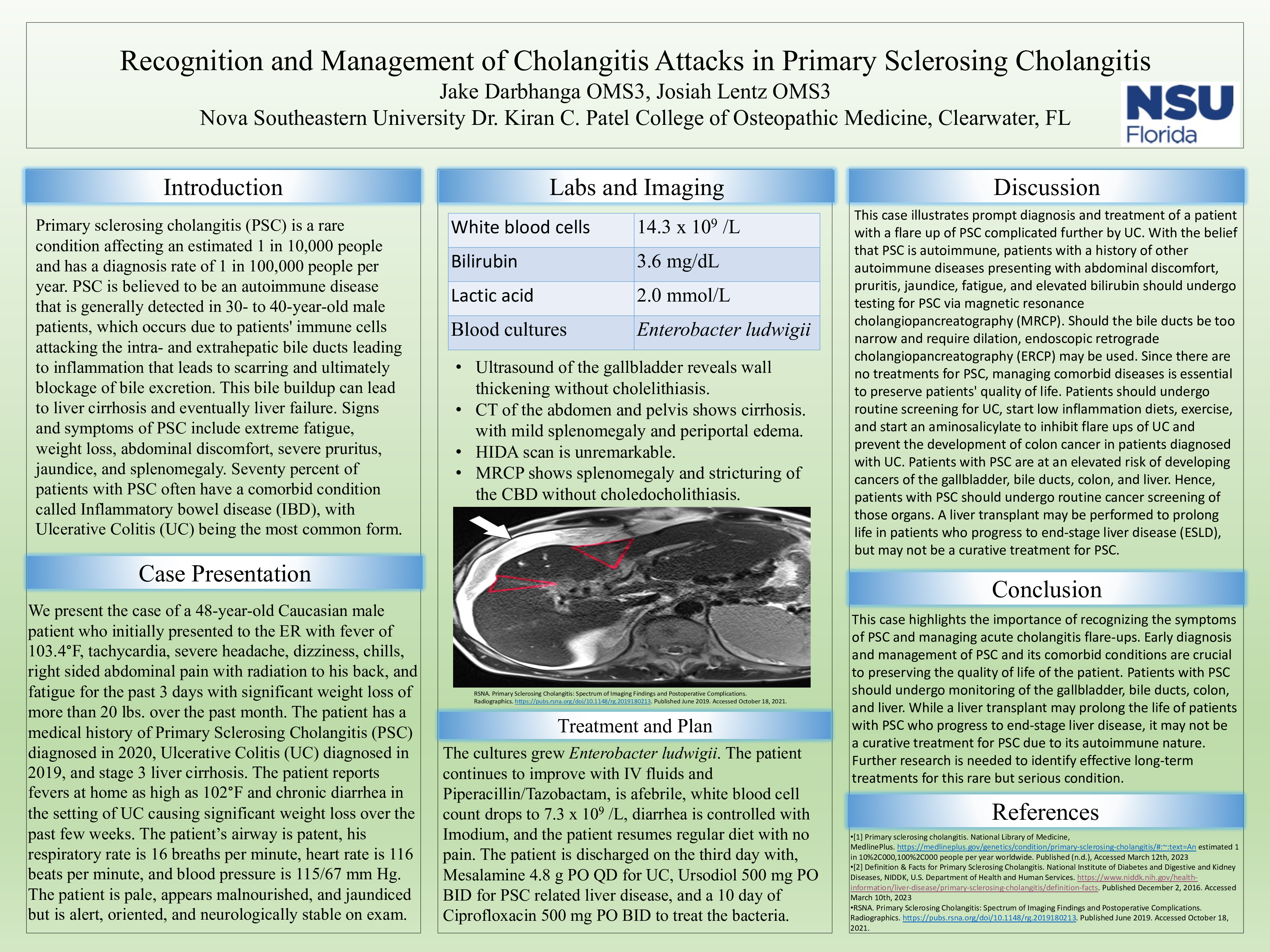
The patient’s airway is patent, respiratory rate is 16 breaths per minute, heart rate is 116 beats per minute, and blood pressure is 115/67 mm Hg. Labs demonstrate white blood cell count of 14.3 x 109 /L, alkaline phosphatase of 401 U/L, bilirubin of 3.6 mg/dL, and lactic acid of 2.0 mmol/L, which meet criteria for sepsis. The patient is pale, appears malnourished, and jaundiced but is alert, oriented, and neurologically stable on exam. Ultrasound of the gallbladder reveals wall thickening without cholelithiasis. MRCP demonstrates splenomegaly without choledocholithiasis. CT of the abdomen and pelvis shows cirrhosis with mild splenomegaly and periportal edema. HIDA scan is unremarkable. Blood cultures are obtained, and the patient is started on Piperacillin/Tazobactam pending further sensitivities as well as parenteral nutrition.
The cultures grew Enterobacter ludwigii. The patient continues to improve with IV fluids and Piperacillin/Tazobactam, is afebrile, white blood cell count drops to 7.3 x 109 /L, diarrhea is controlled with Imodium, and the patient resumes regular diet with no pain. The patient is discharged on the third day with, Mesalamine 4.8 g PO QD for UC, Ursodiol 500 mg PO BID for PSC related liver disease, and a 10 day of Ciprofloxacin 500 mg PO BID to treat the bacteria.
Discussion: This case demonstrates appropriate management of acute flare ups in PSC that are believed to be caused by backup of bile due to inflammation of the intra- and extrahepatic bile ducts, which leads to infection. Keeping the patient stable and treating the bacteria causing the infection is crucial for proper recovery as there is no FDA approved medication to treat PSC.