Abstract
Introduction: Acute cholecystitis is the most common complication of the gallbladder (GB). It has an incidence of around 200,000 cases a year in the United States (US) and affects approximately 20 million individuals in the US. In most cases, it presents with a history of symptomatic gallstones. It is typically resolved with surgery (laparoscopic cholecystectomy) performed within three days of diagnosis. The pathogenesis of acute cholecystitis is most often explained by obstruction of the cystic duct. Research has shown that there are more contributing factors than just obstruction alone. The patient discussed in this case report did not have the most common signs and symptoms of gallbladder disease. The medical team had to rely on additional tests to arrive to the final diagnosis and treatment. This offers an important learning opportunity for future and current healthcare providers. It reminds us of the importance of maintaining a high level of suspicion with each case regardless of how simple it may appear.
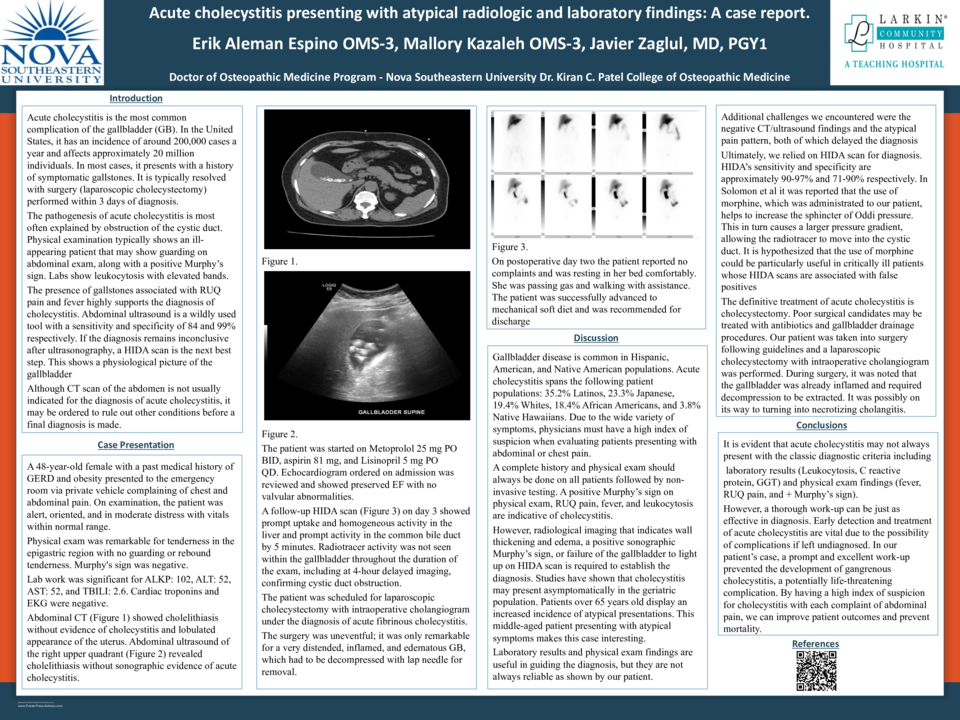
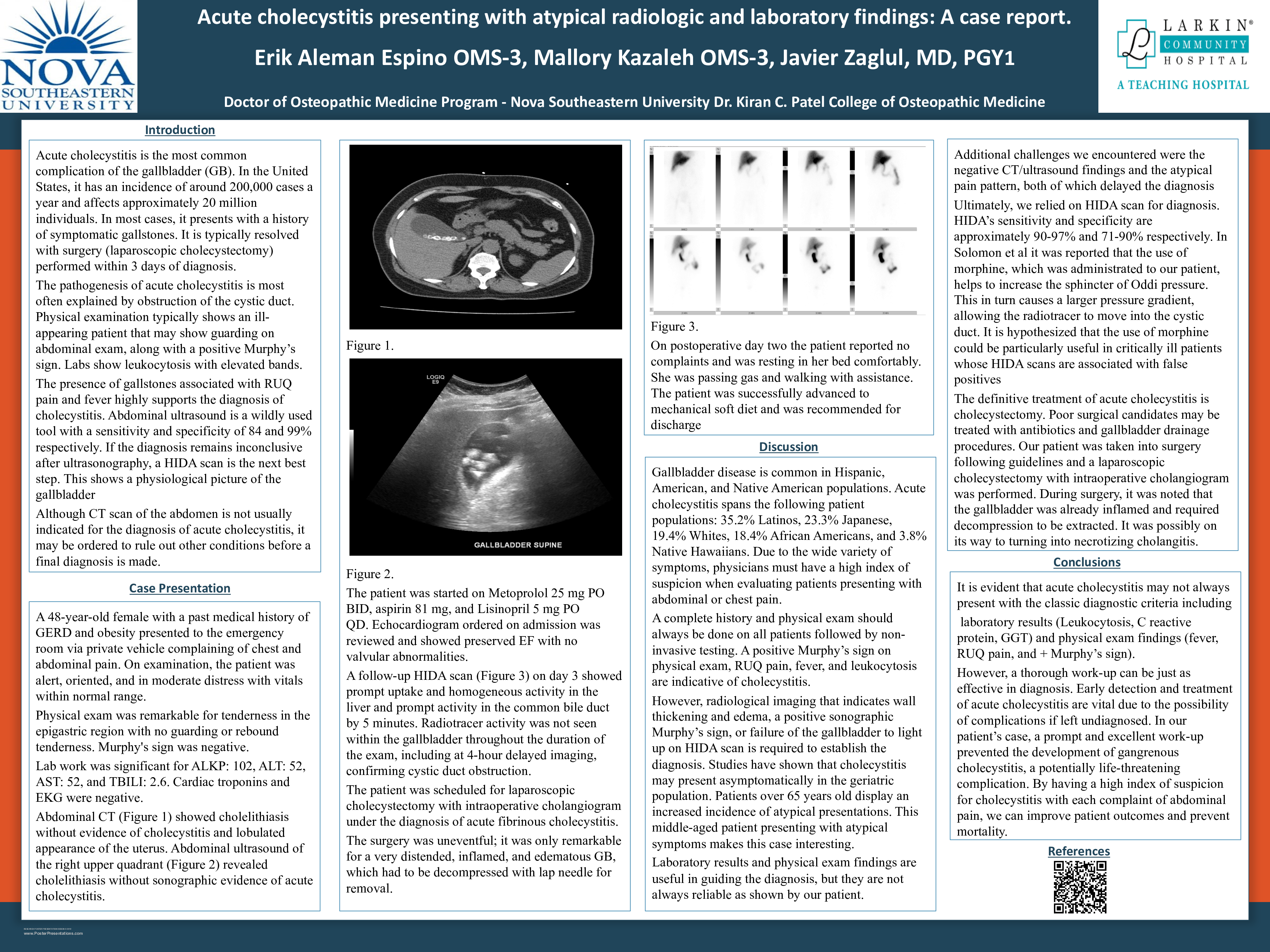
Case Description: We presented a case of a 38-year-old Hispanic woman who presented to our emergency department with a chief complaint of anterior chest wall and epigastric pain. On physical examination, the patient was alert, oriented, and in moderate distress. Vitals: BP: 164/98; Pulse 91; Resp 16; Temp 98.1; Pulse Ox 98%. Negative Murphy's sign. Cardiac troponins and EKG were negative. Initial labs showed no sign of infection with leukocytes within normal range. Liver enzymes were also within normal range on admission. (WBC: 11.0; RBC 4.38; HGB 11.2; ALKP 99; ALT 19; AST 36 TBili 1.3). Follow up abdominal CT scan in the Emergency Department (ED) showed cholelithiasis without evidence of cholecystitis and a lobulated appearance of the uterus. The patient was admitted to the general floor to continue follow up. On day one after admission, the patient continued to display tenderness at the epigastric region without guarding or rebound tenderness. Murphy's sign was still negative. The patient is receiving Morphine 2 mg, but the patient reports persistent mild pain. Abdominal right upper quadrant ultrasound revealed cholelithiasis without sonographic evidence of acute cholecystitis. On day two after admission, the patient was feeling much better. Her pain had improved but she was still reporting some epigastric tenderness. Follow up HIDA scan on day 3 revealed an obstruction of the cystic duct. The patient was scheduled for laparoscopic cholecystectomy with intraoperative cholangiogram. The surgery was uneventful; it was remarkable for a very distended, inflamed, and edematous GB, which had to be decompressed with lap needle for removal. These surgical findings plus the HIDA scan evidence confirmed the diagnosis of acute fibrinous cholecystitis.
Discussion: Our patient in discussion did not exhibit the most common signs and symptoms of gallbladder disease. This case illustrated the importance of maintaining a high index of suspicion for conditions that do not always present with classic signs and symptoms. Delay in diagnosis and treatment of cholecystitis may lead to more severe complications such as gangrenous cholecystitis, which increases risks for complications and mortality.