Abstract
Introduction: Progressive Supranuclear Palsy- Richardson Syndrome (PSP-RS) is an unusual disease that is often misdiagnosed. Although PSP is not considered a rare disease, the prevalence can range between 1.39 to 17.3 cases per 100,000 in the United States. Functional domains including ocular motor dysfunction, postural instability, akinesia, and cognitive dysfunction are core characteristic findings. Common manifestations include early falls from postural instability, supranuclear ophthalmoplegia of vertical gaze, pseudobulbar abnormalities, dystonic rigidity of the upper body, and memory loss. Supportive imaging studies demonstrate atrophy of the brain stem, cerebellum, and basal ganglia, which can be due to neuronal cell loss and associated with neurofibrillary tangles and gliosis. Since PSP shares common pathophysiology and symptoms with other neurodegenerative parkinsonian syndromes, clinical history and imaging should be thoroughly evaluated. PSP-RS has no definitive sex predominance, typically has an onset of symptoms above age 50, and an average disease duration of 5.9 years.
Case Description: This is a case of a 62-year-old Hispanic male with a past medical history of benign prostatic hyperplasia and hypertension who presented with increased rigidity, frequent falls, and loss of balance that started approximately 1 year ago and worsened within the last month. Symptoms started with falls that increased in frequency. The patient’s wife reported his memory started to decline steadily, as well as episodes of dysphagia with associated dysphonia. The patient also reported severe weakness to bilateral upper and lower extremities with reduced facial motor control.
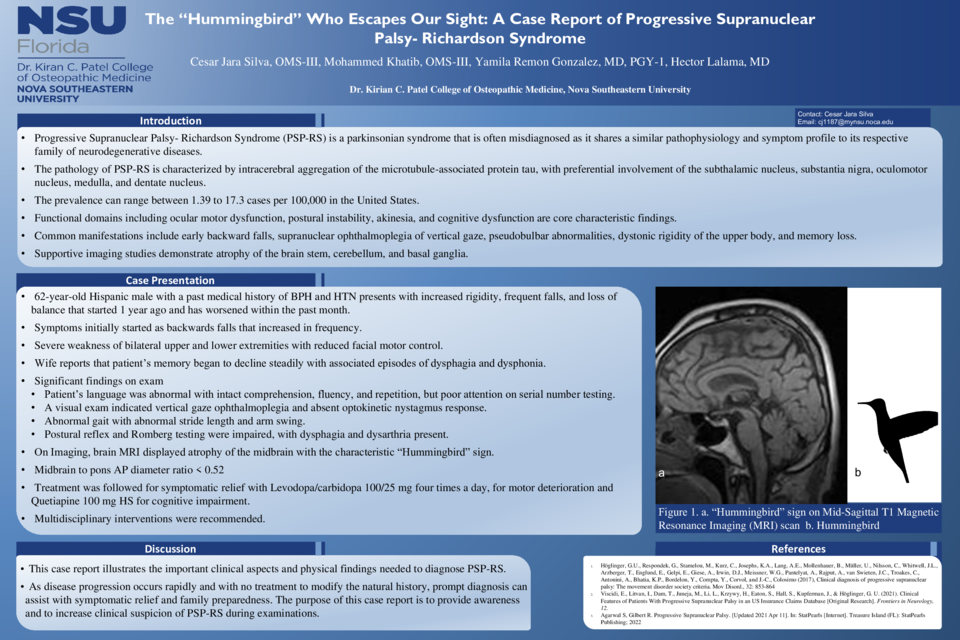
During evaluation, the patient’s language was abnormal with intact comprehension, fluency, and repetition, but poor attention on serial number testing. A visual exam indicated vertical gaze ophthalmoplegia and absent optokinetic nystagmus response. On motor and sensory test, 4+ muscle function on all extremities, and light touch grossly intact in bilateral upper and lower extremities, face, and torso. Reflexes were 3+ symmetrical and Babinski negative. Abnormal gait with abnormal stride length and arm swing was noted. Postural reflex and Romberg testing were impaired, with dysphagia and dysarthria present. For further investigation, an MRI was performed, displaying atrophy of the midbrain with the characteristic “Hummingbird” sign.
Treatment was followed for symptomatic relief with Levodopa/carbidopa 100/25 mg four times a day, for motor deterioration and Quetiapine 100 mg HS for cognitive impairment. Multidisciplinary interventions were recommended, including speech therapy and nutritional counseling that can help manage dysphagia and dysarthria as well as physical therapy for postural instability and falls.
Discussion: This case illustrates the important clinical aspects and physical findings needed to diagnose PSP-RS. As disease progression occurs rapidly and with no treatment to modify the natural history, prompt diagnosis can assist with symptomatic relief and family preparedness. The purpose of this case is to provide awareness and to increase clinical suspicion of PSP-RS during examinations.