Abstract
Background: As simulation-based learning has gained recognition as a means of improving patients’ safety and the quality of care, the demand for simulation has increased exponentially. The same applies for in-situ simulation. This has resulted in a shortage of fully qualified, experienced simulation facilitators.
In-situ simulation has the added benefit of detecting local and system deficiencies, as well as allowing co-workers to learn together.
Finding efficient ways to meet increasing demands, while ensuring the quality of the simulation and learning experience, despite the shortage of experienced facilitators, is there fore of great importance.
Therefore, the purpose was to develop and test semi-standardized simulation scenarios that could be easily adaptable to different hospital units by qualified facilitators.
Method: The choice of scenarios was based on reports from root-cause analysis of adverse events, a review of the most sought-after clinical training opportunities and previous experiences of in-situ simulation. The simulation facilitators will systematically assess the feasibility of use of the scenarios.
Scenarios chosen were:
- Easily adaptable to various units
- Those that require rapid team response
- Scenarios related to rare and/or life threatening situations
- Scenarios influenced by human factors
Learning objectives were:
- Effective teamwork/communication
- Situational/environmental awareness
- Initial assessment with ABCDE approach
- Specific objectives from department/unit
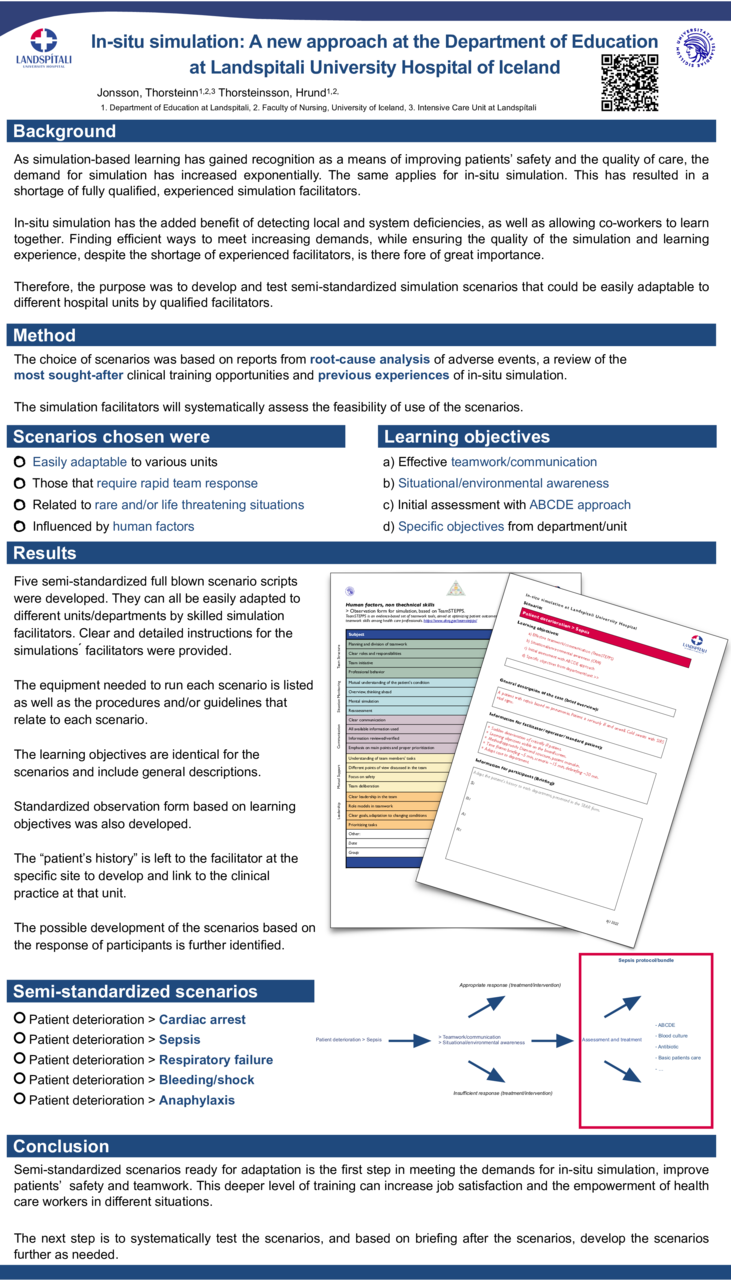
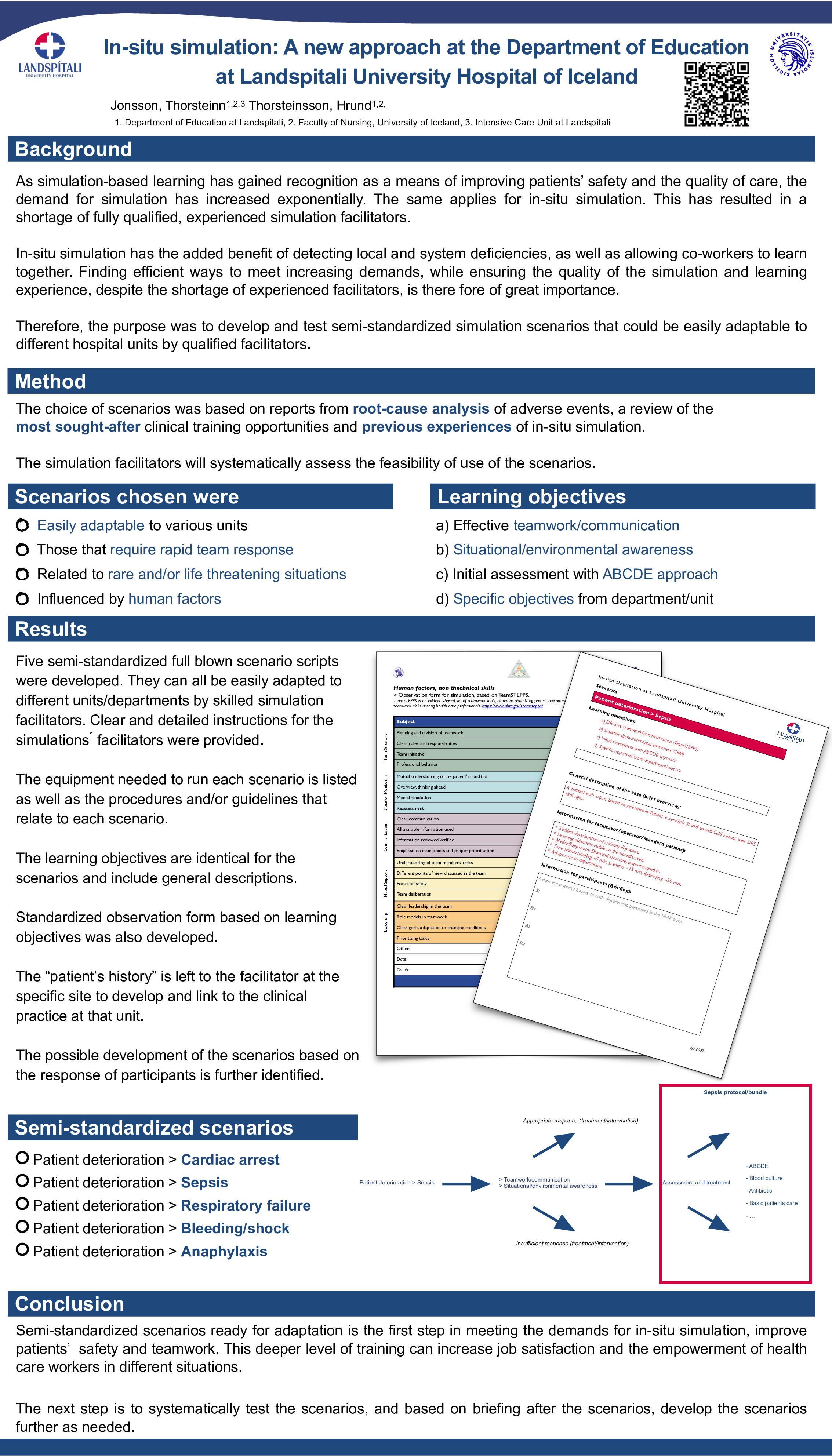
Results: Five semi-standardized full blown scenario scripts were developed. They can all be easily adapted to different units/departments by skilled simulation facilitators. Clear and detailed instructions for the simulations ́ facilitators were provided. The equipment needed to run each scenario is listed as well as the procedures and/or guidelines that relate to each scenario. The learning objectives are identical for the scenarios and include general descriptions. Standardized observation form based on learning objectives was also developed. The “patient’ history” is left to the facilitator at the specific site to develop and link to the clinical practice at that unit. The possible development of the scenarios based on the response of participants is further identified.
Semi-standardized scenarios:
- Patient deterioration > Cardiac arrest
- Patient deterioration > Sepsis
- Patient deterioration > Respiratory failure
- Patient deterioration > Bleeding/shock
- Patient deterioration > Anaphylaxis
Conclusion: Semi-standardized scenarios ready for adaptation is the first step in meeting the demands for in-situ simulation, improve patients’ safety and teamwork. This deeper level of training can increase job satisfaction and the empowerment of health care workers in different situations.
The next step is to systematically test the scenarios, and based on briefing after the scenarios, develop the scenarios further as needed.