Abstract
INTRODUCTION:
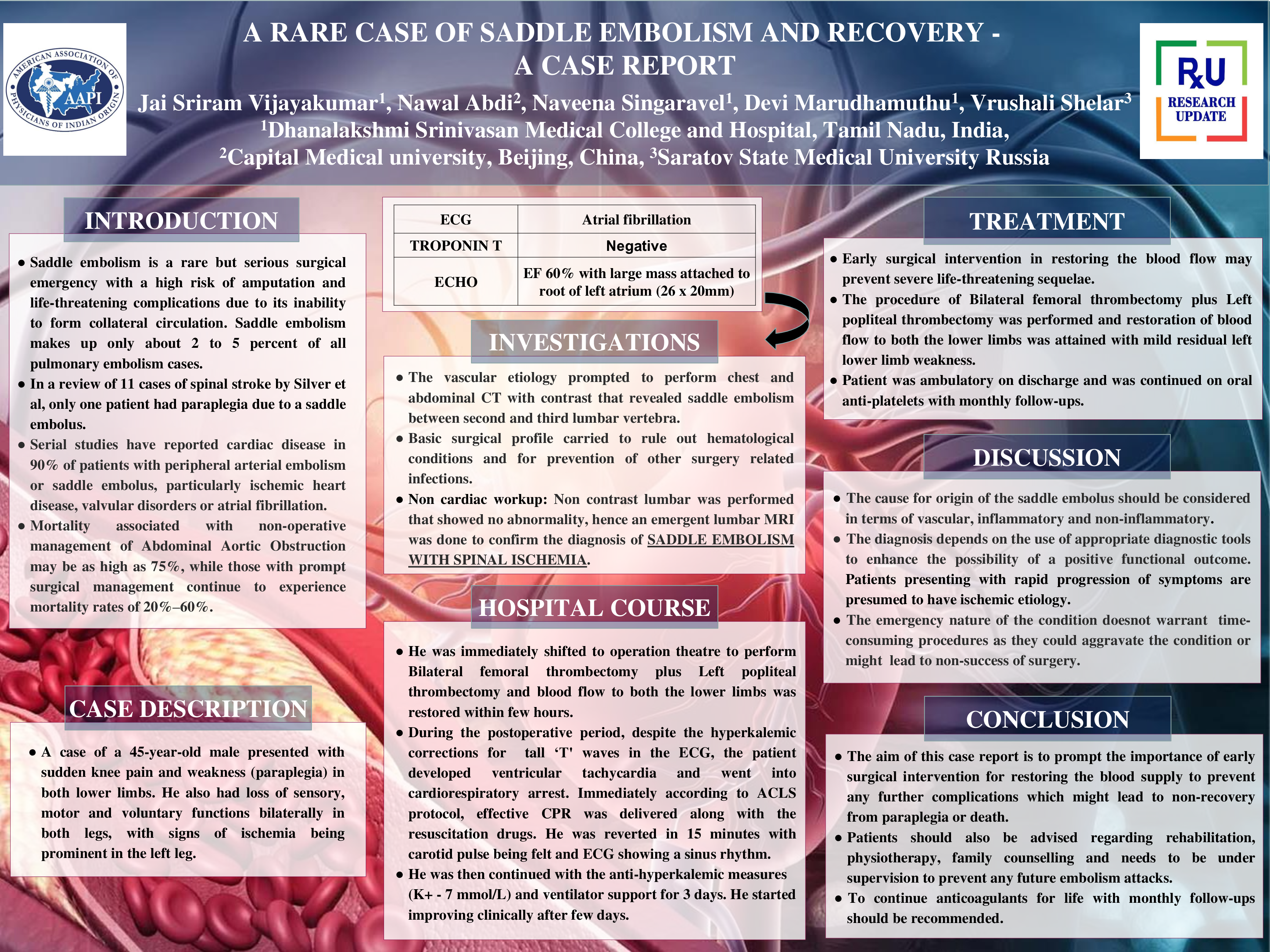
Saddle embolism is a rare but serious surgical emergency with a high risk of amputation and life-threatening complications, as a result of its inability to form collateral circulation.
CASE DESCRIPTION:
A 45-year-old male came into emergency room with symptoms of pain and weakness in the bilateral lower limbs for 10 hours. He was a non-alcoholic and a non-smoker who had no comorbidities except for a right atrial thrombus for which he was treated with 2 doses of low molecular weight heparin from the time of presentation. His vitals showed a pulse rate of 68 beats/minute, blood pressure of 120/80 mmHg, temperature being 98F, and a respiratory rate of 20/minute. Outside reports showed renal and splenic infarcts which was taken on the day of presentation in an outside hospital. He also has a history of recent vaccination of 2nd dose for covid-19 (Covishield). Upon clinical examination, he showed loss of sensory, motor, voluntary functions, and pulsations in both lower limbs. Along with the above findings, his left leg showed skin changes pertaining to ischemia such as shiny, smooth and dry skin. Patient was immediately transferred to operation theatre after doing a doppler study, echo, complete blood count, liver function test, renal function test, APTT, PT-INR, D-dimer, ESR, bleeding time, clotting time, and serology for HIV and hepatitis. Patient underwent, Bilateral femoral thrombectomy and left popliteal thrombectomy and restoration of blood flow to both the lower limbs was attained. Within 1 hour of postoperative period, anti-hyperkalemic measures were initiated for tall ‘T' wave changes in the ECG. Despite the above measures, the patient developed ventricular tachycardia and went into cardiopulmonary arrest. Immediately according to ACLS protocol, effective CPR was delivered along with the delivery of the resuscitation drugs. He was reverted to sinus rhythm in 15 minutes with carotid pulse being felt. He was then continued with the anti-hyperkalemic measures since his arterial blood gas showed potassium levels of around 7 mmol/L. He was on ventilator support for few days and then his condition started improving clinically. He was advised to continue the anticoagulants with monthly follow-ups after discharge.
CONCLUSION:
The significance of this case report is to make an early surgical intervention for restoring the blood supply and preventing any further complications which might lead to non-recovery from paraplegia or death. Patients should also be advised regarding rehabilitation, physiotherapy, family counselling and needs to be under supervision to prevent any future embolism attacks.