Abstract
Case Description: We present a 54-year-old previously healthy male with a two-month history of decreased vision at all ranges and blurred vision that progressively worsened. The patient denied pain or discomfort but complained of bothersome glare and brightness. A dislocated intraocular lens was observed in the right eye upon slit-lamp examination. Double vision was reported due to the lower positioning of the lens. Previous ocular history included bilateral primary open-angle glaucoma, weak ciliary zonules, and lens replacement of the left eye. There was no family history of ocular disease. A review of systems was negative, and medical and social history was noncontributory. The external eye exam was normal. Visual acuity with correction was 20/100 OD and 20/30 OS. The ocular exam showed pupils equal, round, and reactive to light and accommodation. Extraocular motility showed a full range of motion. Slit-lamp examination was remarkable for >180 degrees of zonular dehiscence OD. PCIOL OS was centered. IOP was 22 in both eyes. The fundus exam was normal.
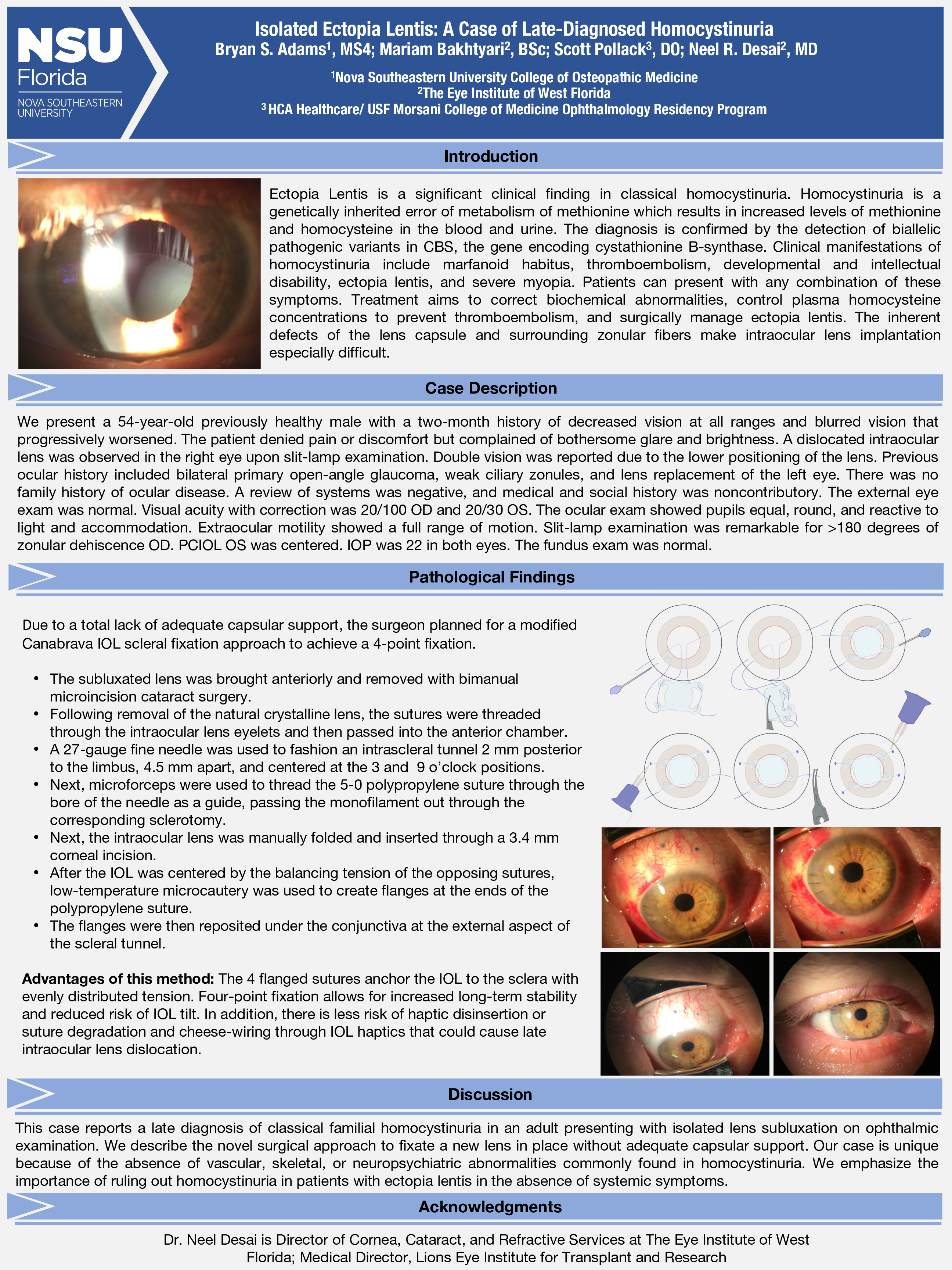
Surgical Approach: Due to a total lack of adequate capsular support, the surgeon planned for a modified Canabrava IOL scleral fixation approach to achieve a 4-point fixation. First, the subluxated lens was brought anteriorly and removed with bimanual microincision cataract surgery. Following removal of the natural crystalline lens, the sutures were threaded through the intraocular lens eyelets and then passed into the anterior chamber. A 27-gauge fine needle was used to fashion an intrascleral tunnel 2 mm posterior to the limbus, 4.5 mm apart, and centered at the 3 and 9 o’clock positions. Next, microforceps were used to thread the 5-0 polypropylene suture through the bore of the needle as a guide, passing the monofilament out through the corresponding sclerotomy. Next, the intraocular lens was manually folded and inserted through a 3.4 mm corneal incision. After the IOL was centered by balancing the tension of the opposing sutures, low-temperature microcautery was used to create flanges at the ends of the polypropylene suture. The flanges were then reposited under the conjunctiva at the external aspect of the scleral tunnel. The 4-flanged sutures anchor the IOL to the sclera with evenly distributed tension. Four-point fixation allows for increased long-term stability and reduced risk of IOL tilt. In addition, there is less risk of haptic disinsertion or suture degradation and cheese-wiring through IOL haptics that could cause late intraocular lens dislocation.
Discussion: This case reports a late diagnosis of classical familial homocystinuria in an adult presenting with isolated lens subluxation on ophthalmic examination. We describe the novel surgical approach to fixate a new lens in place without adequate capsular support. Our case is unique because of the absence of vascular, skeletal, or neuropsychiatric abnormalities commonly found in homocystinuria. We emphasize the importance of ruling out homocystinuria in patients with ectopia lentis in the absence of systemic symptoms.