Abstract
Background: Disseminated intravascular coagulation (DIC) is a serious condition that involves extreme blood clotting due to the body’s response to another disease or infection. Although a rare condition, the body over activates excessive clotting mechanisms while trying to fight off the primary illness, resulting in thrombus formation. As clotting factors are used up, the body is unable to respond to stop any additional bleeding that may occur, increasing risk of hemorrhage and organ failure. DIC occurs in patients with severe infection or inflammation, such as sepsis, trauma, pregnancy complications and cancer. As pregnancy and sepsis do not apply the pediatric population with much frequency, DIC is more likely to occur due to malignancy. The rarity of DIC has resulted in few studies exploring how it affects the pediatric population, especially pediatrics with cancer. This study aimed to fill that gap in determining outcomes of DIC on oncologic pediatric patients.
Objective: The goal of this study was to investigate the determination of clinical outcomes of oncologic pediatric patients who acquire disseminated intravascular coagulation.
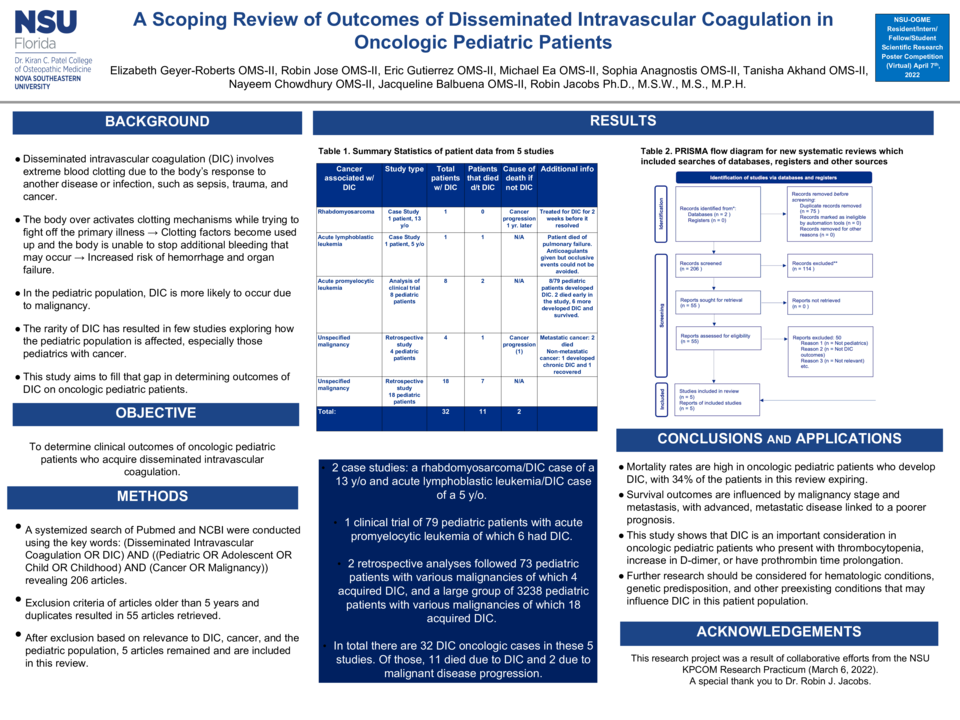
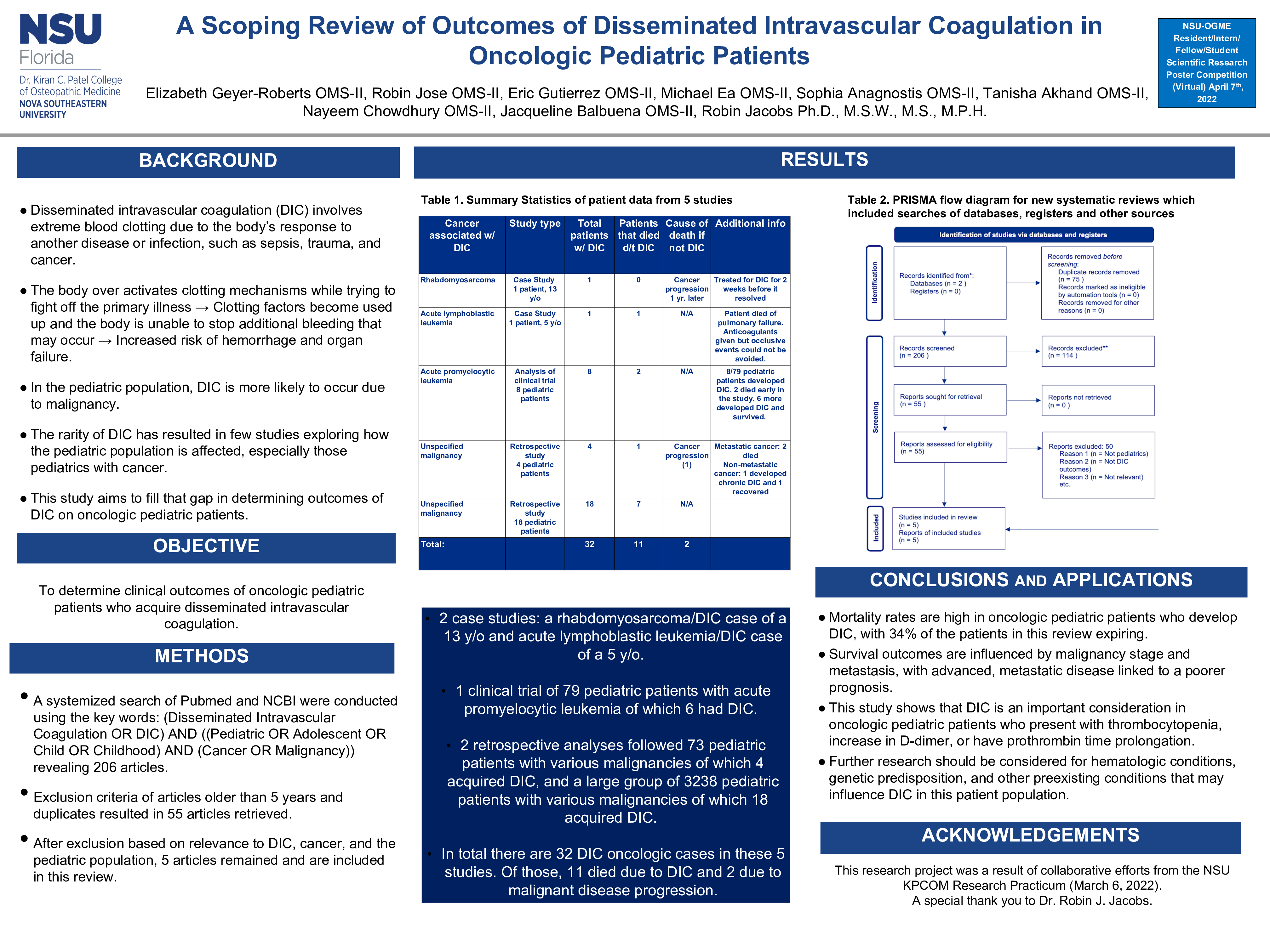
Methods: A systemized search of the databases PubMed and NCBI was conducted using the key words: (Disseminated Intravascular Coagulation OR DIC) AND ((Pediatric OR Adolescent OR Child OR Childhood) AND (Cancer OR Malignancy)) yielding 206 articles. Articles were included if they were published withing the past 5 years and were in the English language. After removing duplicates and screening articles based on their relevance to DIC, cancer and the pediatric population, five articles remained and are included in this review.
Results: Of the five articles included there were two case studies, one clinical trial analysis, and two retrospective data studies. The case studies were a rhabdomyosarcoma/DIC case of a 13-year-old and acute lymphoblastic leukemia/DIC case of a 5-year-old. In the five articles, 32 DIC oncologic cases were discussed; of those, 11 died due to DIC and 2 died due to malignant disease progression. Of those who develop DIC, mortality rates are high, with 34% of the patients in this review expiring. The results suggest that survival outcomes are influenced by malignancy stage and metastasis, with advanced, metastatic disease linked to a poorer prognosis. Additionally, an ISTH DIC score ≥ 6 and WBC were associated with early death and significant coagulopathy events. However, neither marker was specific/sensitive enough to be considered reliable so other markers should be considered for research.
Conclusion: While DIC remains uncommon in the overall oncologic pediatric population, it should remain a consideration, especially in those who present with thrombocytopenia, increase in D-dimer, or have prothrombin time prolongation. Further research should also be considered for hematologic conditions, genetic predisposition, and other preexisting conditions that may influence DIC in this patient population.