Abstract
Laryngeal carcinoma is a less common form of cancer worldwide, making up about 1.0% of all new cancer cases in 2020. The strongest risk factors associated with this form of cancer are tobacco and alcohol use with over 95% of patients having reported use. The most common histology seen in approximately 95% of cases of laryngeal carcinoma is squamous cell carcinoma. Other malignancies that commonly metastasize to the larynx include cutaneous melanoma, renal cell carcinoma, breast carcinoma and lung carcinoma.
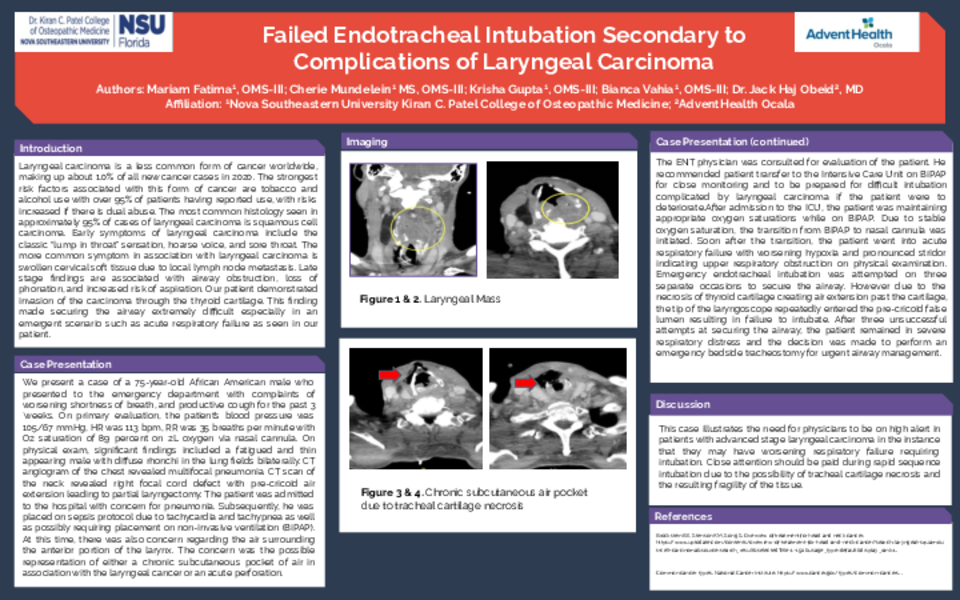
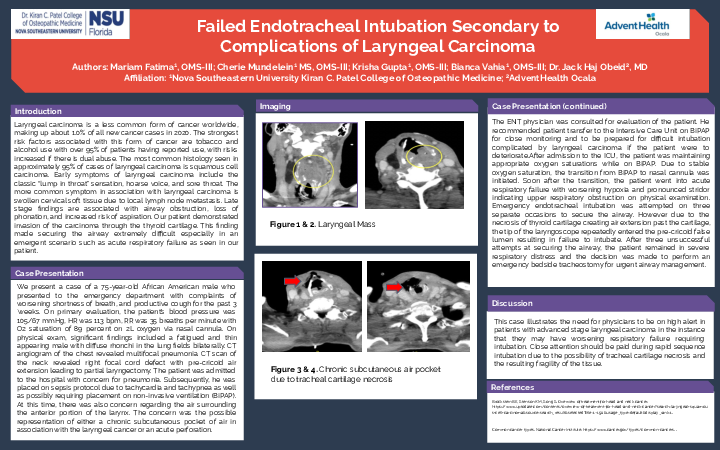
Case Description: We present a case of a 75-year-old male who presented to the emergency department with complaints of worsening shortness of breath, and productive cough for the past three weeks. On primary evaluation, the patient’s blood pressure was 105/67 mmHg, heart rate was 113 beats per minute, respiratory rate was 35 breaths per minute with oxygen saturation of 89 percent on two liters of oxygen via nasal cannula. On physical exam, significant findings included a fatigued and thin appearing male with diffuse rhonchi in the lung fields bilaterally. Imaging in the emergency department included a CT angiogram of the chest and CT scan of the neck. CT angiogram of the chest revealed multifocal pneumonia. CT scan of the neck revealed right focal cord defect with pre-cricoid air extension leading to partial laryngectomy.
The patient was admitted to the hospital with concern for pneumonia. Subsequently, he was placed on sepsis protocol due to tachycardia and tachypnea as well as possibly requiring placement on non-invasive ventilation (BiPAP). At this time, there was also concern regarding the air surrounding the anterior portion of the larynx. The concern was the possible representation of either a chronic subcutaneous pocket of air in association with the laryngeal cancer or an acute perforation. The ENT physician was consulted for evaluation of the patient. He recommended patient transfer to the Intensive Care Unit on BiPAP for close monitoring and to be prepared for difficult intubation complicated by laryngeal carcinoma if the patient were to deteriorate.
After admission to the ICU, the patient was maintaining appropriate oxygen saturations while on BiPAP. Due to stable oxygen saturation, the transition from BiPAP to nasal cannula was initiated. Soon after the transition, the patient went into acute respiratory failure with worsening hypoxia and pronounced stridor indicating upper respiratory obstruction on physical examination. Emergency endotracheal intubation was attempted on three separate occasions to secure the airway. However due to the necrosis of thyroid cartilage creating air extension past the cartilage, the tip of the laryngoscope repeatedly entered the pre-cricoid false lumen resulting in failure to intubate. After three unsuccessful attempts at securing the airway, the patient remained in severe respiratory distress and the decision was made to perform an emergency bed-side tracheostomy for urgent airway management.
Discussion: This case illustrates the need for physicians to be on high alert in patients with advanced stage laryngeal carcinoma in the instance that they may have worsening respiratory failure requiring intubation. Close attention should be paid during rapid sequence intubation due to the possibility of tracheal cartilage necrosis and the resulting fragility of the tissue.