Abstract
Introduction: Limited joint mobility in diabetes mellitus, formerly known as diabetic cheiroarthropathy, results from thickening of the dermis and fibrosis of subcutaneous tissue due to excessive glycosylation of collagen in nearly all joints, most commonly affecting the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints of the hands.5,9
Patients with limited joint mobility present with painless stiffness and decreased grip strength with a history of diabetes.5 Additionally, they may complain of decreasing ability to complete fine movements and maintenance of general hand function.5 Associated with joint stiffness may be a thickened and waxy appearance of the skin, particularly on the dorsum of the fingers; this is known as diabetic sclerodactyly.5 In addition to the PIP and MCP joints, the wrists, elbows, shoulders, knees, feet, and components of the axial skeleton may be limited in mobility as well.5
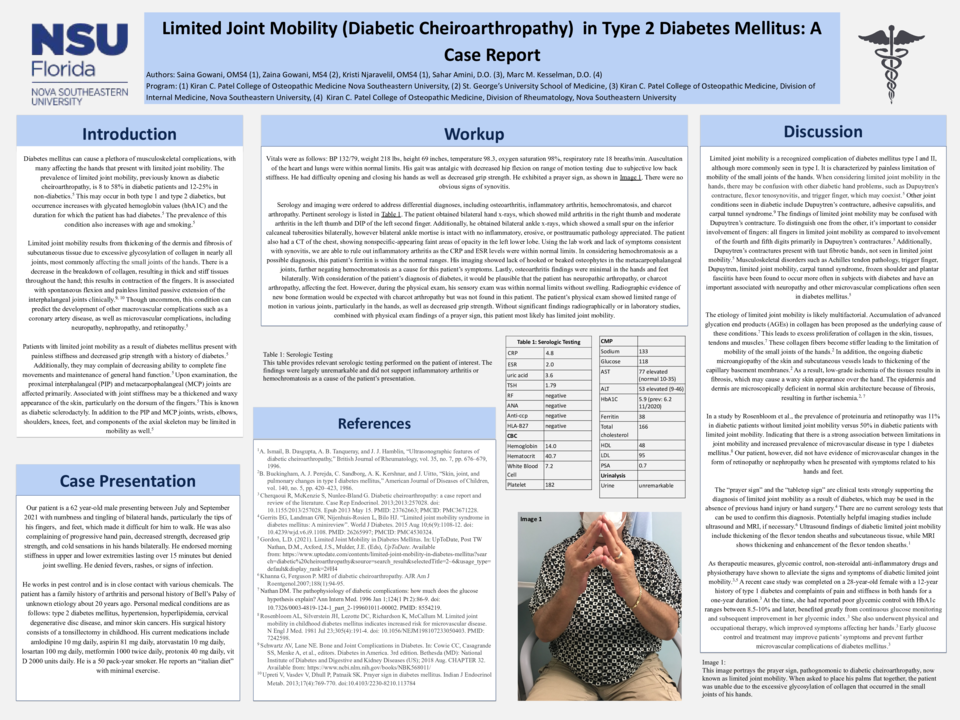
Case Description: A 62 year-old male presented to the outpatient clinic between July and September 2021 with numbness and tingling of bilateral hands that began several years ago. This affected the tips of his fingers and feet in particular, making it difficult for him to walk. He also complained of progressive hand pain, decreased strength, decreased grip strength, and cold sensations in his hands bilaterally. He endorsed morning stiffness in upper and lower extremities lasting over 15 minutes but denied joint swelling. He denied fevers, rashes, or signs of infection. Personal medical conditions are as follows: type 2 diabetes mellitus, hypertension, hyperlipidemia, cervical degenerative disc disease, and minor skin cancers. His gait was antalgic with decreased hip flexion on range of motion testing due to subjective low back stiffness. He had difficulty opening and closing his hands as well as decreased grip strength. He exhibited a prayer sign without obvious signs of synovitis.
Discussion: Limited joint mobility is a recognized complication of diabetes mellitus type I and II, although more commonly seen in type I.5 The etiology of limited joint mobility is likely multifactorial. Accumulation of advanced glycation end products (AGEs) in collagen has been proposed as the underlying cause of these conditions.7 This leads to excess proliferation of collagen in the skin, tissues, tendons and muscles.7 These collagen fibers become stiffer leading to the limitation of mobility of the small joints of the hands.2 In addition, the ongoing diabetic microangiopathy of the skin and subcutaneous vessels leads to thickening of the capillary basement membranes.2 As a result, low-grade ischemia of the tissues can cause fibrosis, which may produce a waxy skin appearance over the hand.2,7 The “prayer sign” and the “tabletop sign” are clinical tests strongly supporting the diagnosis of limited joint mobility.4, 5 There are no current serology tests that can be used to confirm this diagnosis. Potentially helpful imaging studies include ultrasound and MRI, if necessary.6 As therapeutic measures, glycemic control, non-steroidal anti-inflammatory drugs and physiotherapy have shown to alleviate the signs and symptoms of limited joint mobility.5 Early glucose control and treatment may improve patients’ symptoms and prevent further microvascular complications of diabetes mellitus.5