Abstract
Introduction – Colorectal cancer (CRC) is the fourth most diagnosed cancer in the country. Screening begins at the age of 45 years in patients who are not high-risk. Risk factors include family history, hereditary syndromes, diet, and several conditions such as IBD and obesity. Symptoms are usually non-specific, but may include changes in bowel habits, abdominal pain, GI bleeds, and weight loss. Colonoscopy with histology is diagnostic for CRC. Staging of the neoplasm is necessary for managing the patient’s course. Surgical resection of colorectal cancers and metastases is curative. For CRC staged as 2 or greater, chemotherapy and/or radiation is required. All patients with CRC need to be monitored for possible recurrence.
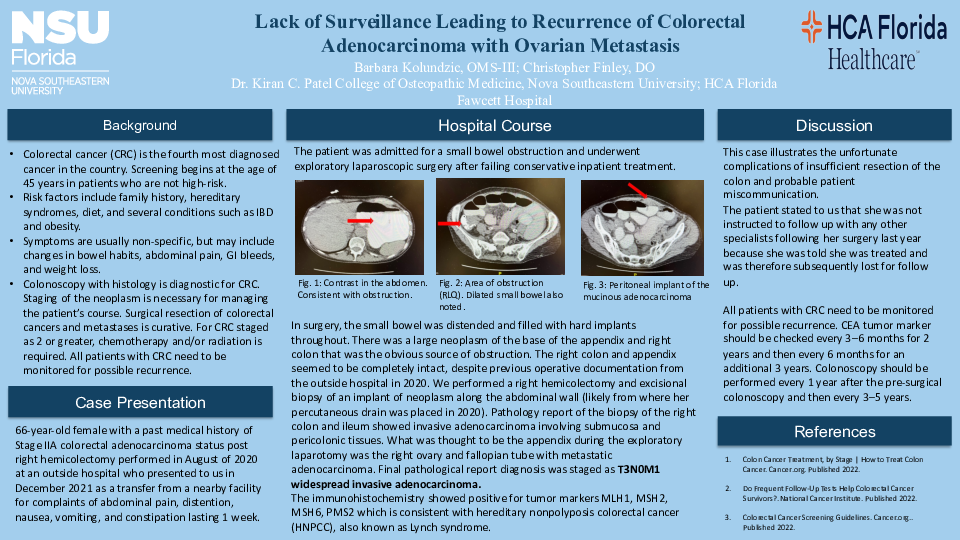
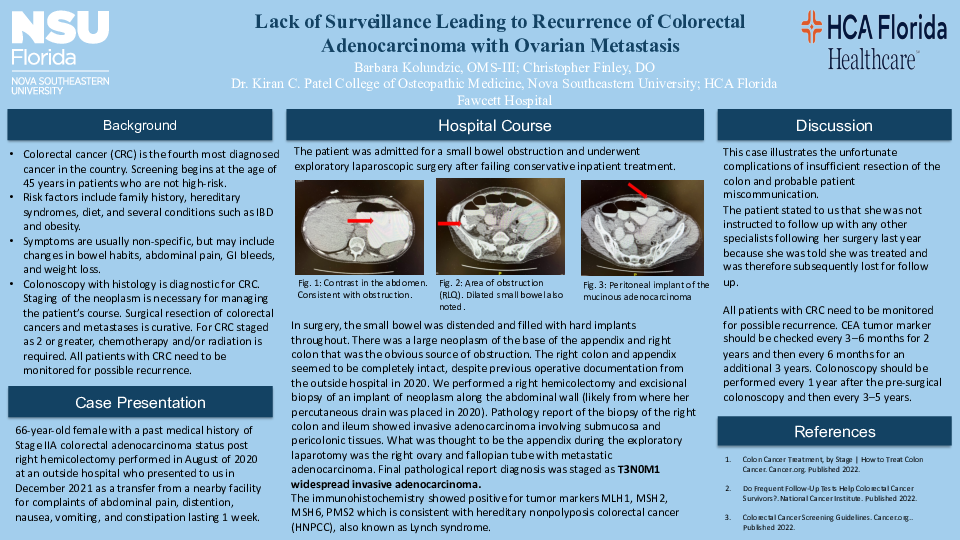
Case Description – A 66-year-old female with a past medical history of Stage IIA colorectal adenocarcinoma status post right hemicolectomy performed in August of 2020 at an outside hospital who presented to us in December 2021 as a transfer from a nearby facility for complaints of abdominal pain, distention, nausea, vomiting, and constipation lasting 1 week. She was admitted for a small bowel obstruction and underwent exploratory laparoscopic surgery after failing conservative inpatient treatment. In surgery, the small bowel was distended down to the level of the terminal ileum and filled with hard implants throughout. There was a large mucinous appearing neoplasm of the base of the appendix and right colon that was causing an apple-core lesion and the obvious source of obstruction. The right colon and appendix seemed to be completely intact, despite previous operative documentation from the outside hospital in 2020. We performed a right hemicolectomy and excisional biopsy of an implant of neoplasm along the abdominal wall (likely from where her percutaneous drain was placed in 2020). Pathology report of the biopsy of the right colon and ileum showed invasive adenocarcomina involving submucosa and pericolonic tissues. What was thought to be the appendix during the exploratory laparotomy was the right ovary and fallopian tube with metastatic adenocarcinoma. Final pathological report diagnosis was staged as T3N0M1 widespread invasive adenocarcinoma.
Discussion – Upon review of prior medical records, pathology reports from the hemicolectomy that was performed in 2020 showed Grade 2 moderately differentiated adenocarcinoma of the cecum. “The distal segment of terminal ileum measuring 6.7 cm in length. The attached cecum and proximal segment of ascending colon measuring 9.5 cm in length. Appendix shows a severely congested serosa and dilated appendiceal lumen.” The immunohistochemistry showed positive for tumor markers MLH1, MSH2, MSH6, PMS2 which is consistent with hereditary nonpolyposis colorectal cancer (HNPCC), also known as Lynch syndrome. The patient stated to us that she was not instructed to follow up with any other specialists following her surgery last year because she was told she was treated and was therefore subsequently lost for follow up. All patients with CRC need to be monitored for possible recurrence. CEA tumor marker should be checked every 3–6 months for 2 years and then every 6 months for an additional 3 years. Colonoscopy should be performed every 1 year after the pre-surgical colonoscopy and then every 3–5 years. This case illustrates the unfortunate complications of insufficient resection of the colon and probable patient miscommunication.