Abstract
INTRODUCTION: Radiation therapy in advanced gynecological cancer remains as an important aspect in the management of the disease. Gynecological cancer either cervical and or uterine present a profound challenge to the treating team when presenting with bulky and advanced disease. Although many improvements have been made through refinements in standard-of-care management, including more conformal external radiation options, the addition of concurrent chemotherapy to radiotherapy, and advances in image guided brachytherapy, the outcome for far-advanced bulky tumors is poor. In these patients with few radiation therapy options, because of residual, bulky, recurrent or metastatic disease radiosurgery has shown promise in improving local tumor control while toxicity remains low.
OBJECTIVES
- To describe the use of stereotactic body radiotherapy (SBRT) in gynecological cancers.
- To evaluate toxicity, local control, and overall survival in patients with gynecological cancer treated using radiosurgery
INDICATIONS
SBRT for Metastatic disease
SBRT for Recurrent disease
SBRT Boost
- Before EBRT
- After EBRT (residual mass, VC, enlarged LN)
- As an Alternative to Brachytherapy
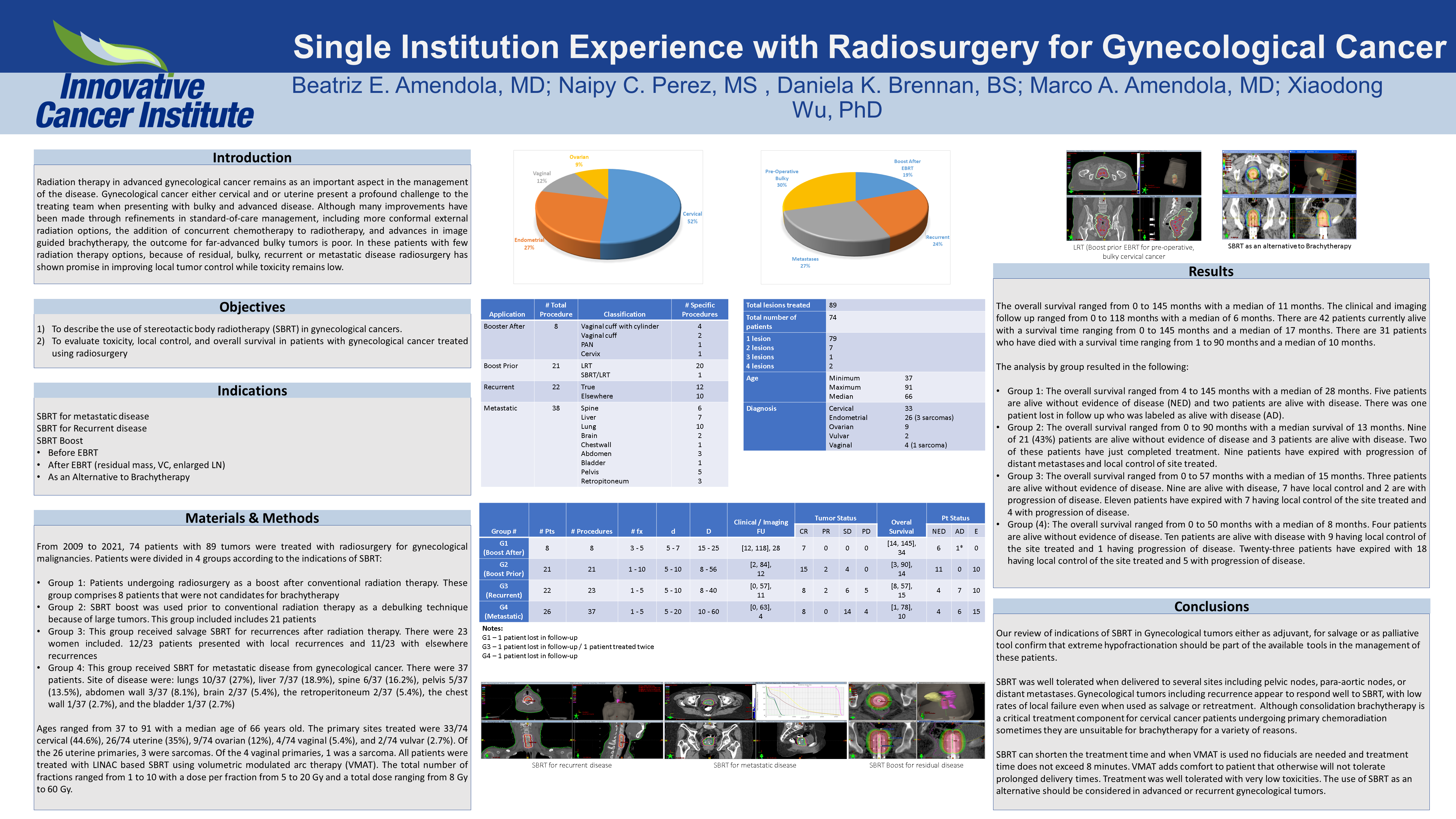
MATERIALS & METHODS: From 2009 to 2021, 74 patients with 89 tumors were treated with radiosurgery for gynecological malignancies. Patients were divided in 4 groups according to the indications of SBRT:
- Group 1: Patients undergoing radiosurgery as a boost after conventional radiation therapy. This group comprises 8 patients that were not candidates for brachytherapy
- Group 2: SBRT boost was used prior to conventional radiation therapy as a debulking technique because of large tumors. This group included includes 21 patients
- Group 3: This group received salvage SBRT for recurrences after radiation therapy. There were 23 women included. 12/23 patients presented with local recurrences and 11/23 with elsewhere recurrences
- Group 4: This group received SBRT for metastatic disease from gynecological cancer. There were 37 patients. Site of disease were: lungs 10/37 (27%), liver 7/37 (18.9%), spine 6/37 (16.2%), pelvis 5/37 (13.5%), abdomen wall 3/37 (8.1%), brain 2/37 (5.4%), the retroperitoneum 2/37 (5.4%), the chest wall 1/37 (2.7%), and the bladder 1/37 (2.7%)
Ages ranged from 37 to 91 with a median age of 66 years old. The primary sites treated were 33/74 cervical (44.6%), 26/74 uterine (35%), 9/74 ovarian (12%), 4/74 vaginal (5.4%), and 2/74 vulvar (2.7%). Of the 26 uterine primaries, 3 were sarcomas. Of the 4 vaginal primaries, 1 was a sarcoma. All patients were treated with LINAC based SBRT using volumetric modulated arc therapy (VMAT). The total number of fractions ranged from 1 to 10 with a dose per fraction from 5 to 20 Gy and a total dose ranging from 8 Gy to 60 Gy.
RESULTS: The overall survival ranged from 0 to 145 months with a median of 11 months. The clinical and imaging follow-up ranged from 0 to 118 months with a median of 6 months. There are 42 patients currently alive with a survival time ranging from 0 to 145 months and a median of 17 months. There are 31 patients who have died with a survival time ranging from 1 to 90 months and a median of 10 months.
The analysis by group resulted in the following:
- Group 1: The overall survival ranged from 4 to 145 months with a median of 28 months. Five patients are alive without evidence of disease (NED) and two patients are alive with disease. There was one patient lost in follow-up who was labeled as alive with disease (AD).
- Group 2: The overall survival ranged from 0 to 90 months with a median survival of 13 months. Nine of 21 (43%) patients are alive without evidence of disease and 3 patients are alive with disease. Two of these patients have just completed treatment. Nine patients have expired with progression of distant metastases and local control of site treated.
- Group 3: The overall survival ranged from 0 to 57 months with a median of 15 months. Three patients are alive without evidence of disease. Nine are alive with disease, 7 have local control and 2 are with progression of disease. Eleven patients have expired with 7 having local control of the site treated and 4 with progression of disease.
- Group (4): The overall survival ranged from 0 to 50 months with a median of 8 months. Four patients are alive without evidence of disease. Ten patients are alive with disease with 9 having local control of the site treated and 1 having progression of disease. Twenty-three patients have expired with 18 having local control of the site treated and 5 with progression of disease.
CONCLUSIONS: Our review of indications of SBRT in Gynecological tumors either as adjuvant, for salvage or as palliative tool confirm that extreme hypofractionation should be part of the available tools in the management of these patients.
SBRT was well tolerated when delivered to several sites including pelvic nodes, para-aortic nodes, or distant metastases. Gynecological tumors including recurrence appear to respond well to SBRT, with low rates of local failure even when used as salvage or retreatment. Although consolidation brachytherapy is a critical treatment component for cervical cancer patients undergoing primary chemoradiation sometimes they are unsuitable for brachytherapy for a variety of reasons.
SBRT can shorten the treatment time and when VMAT is used no fiducials are needed and treatment time does not exceed 8 minutes. VMAT adds comfort to patient that otherwise will not tolerate prolonged delivery times. Treatment was well tolerated with very low toxicities. The use of SBRT as an alternative should be considered in advanced or recurrent gynecological tumors.