Abstract
Background:
Melioidosis is caused by Burkholderia pseudomallei which is a gram-negative bacterium. It is an environmental saprophyte found in wet soils. It is a rare disease in the general population but mostly infects adults with an underlying predisposing condition, mainly diabetes mellitus, and immunocompromised individuals. Also, farmers who have an associated immunocompromised condition are more likely to acquire this disease. The average annual incidence of melioidosis was 12.3 per 100000 population. It has a high mortality rate when untreated and hence the diagnosis and management require high clinical suspicion along with other microbiological techniques.
Case presentation:
A 35-year-old male who is a known case of diabetes and chronic alcoholism, presented with complaints of back pain and multiple joint pain associated with swelling for the past 15 days. He had a history of recurrent febrile illness associated with polyarthritis, osteomyelitis of the right elbow, and an abscess which was followed by an ulcer in the left supraclavicular region for which he was treated with empirical Anti-tubercular drugs for 1 year due to clinical suspicion of Tuberculosis. On evaluation, the patient was disoriented, icteric, febrile (40°C), and with abdominal distension. The patient was in respiratory distress with vitals being suggestive of shock.
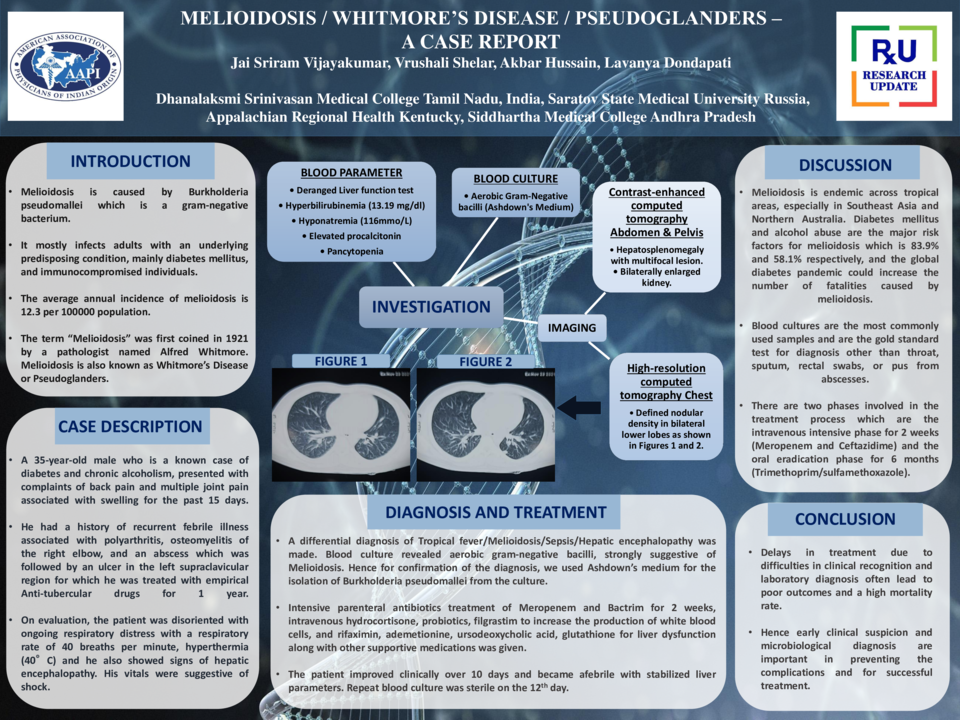
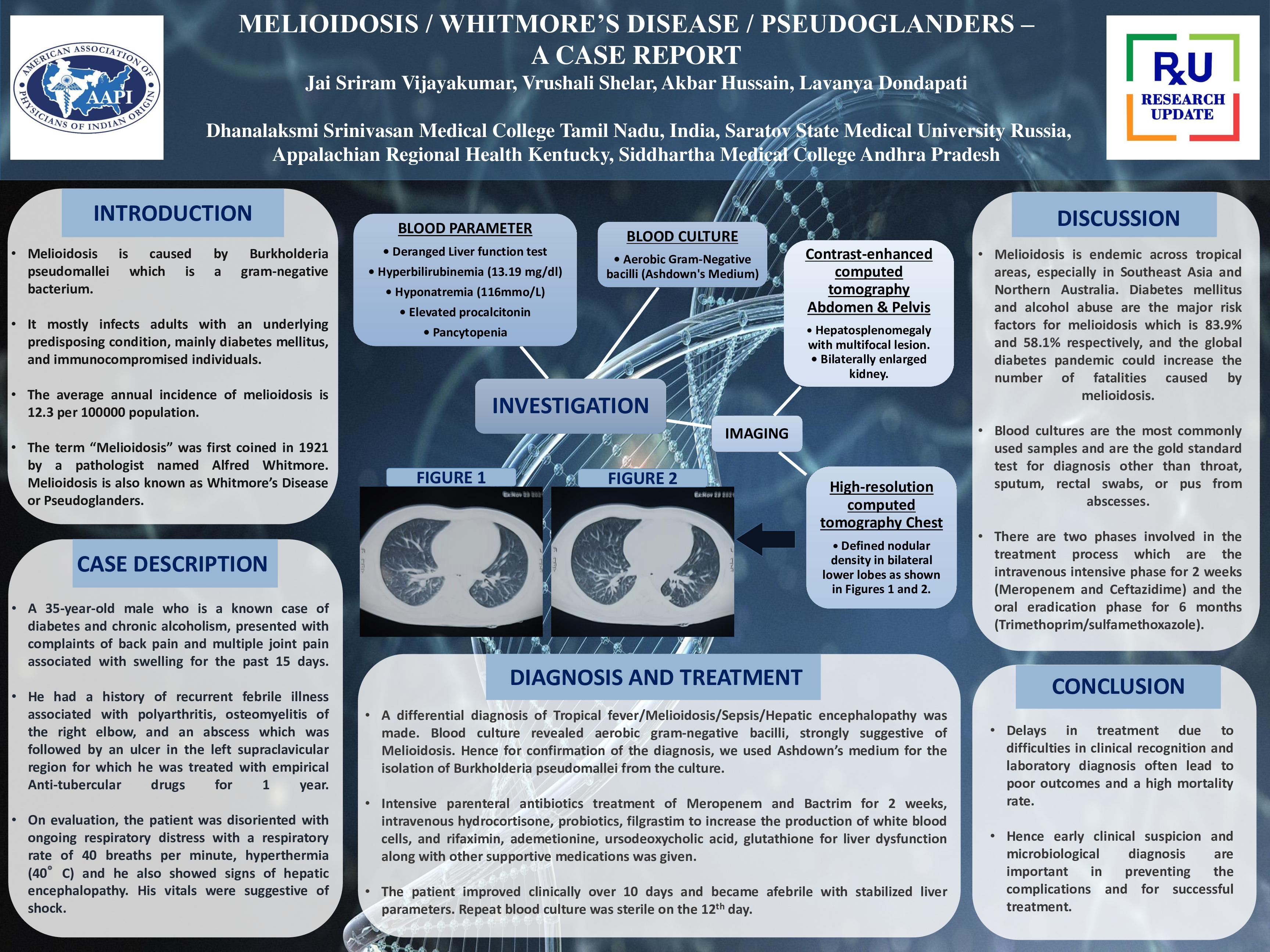
Blood investigations showed a deranged liver function test of increase in SGOT, bilirubin (13.19 mg/dL), hypoalbuminemia (2.1 g/dL), hyponatremia (116 mmol/L), pancytopenia with elevated procalcitonin, and C-reactive protein. Contrast-enhanced computed tomography of abdomen & pelvis showed hepatosplenomegaly with multifocal lesions and bilaterally enlarged kidneys. A High-resolution computed tomography chest showed well-defined nodular density in the right upper and bilateral lower lobes.
A differential diagnosis of Tropical fever/Melioidosis/Sepsis/Hepatic encephalopathy was made. The patient was started on broad-spectrum antibiotics after sending blood and urine cultures. Blood culture revealed aerobic gram-negative bacilli, strongly suggestive of Melioidosis. Hence for confirmation of the diagnosis, we used Ashdown’s medium for the isolation of Burkholderia pseudomallei from the culture. A final diagnosis of disseminated melioidosis was made by culture-positive results for Burkholderia pseudomallei and its widespread clinical symptoms involving multiple organs.
Intensive parenteral antibiotics treatment of Meropenem and Bactrim for 2 weeks, intravenous hydrocortisone, probiotics, filgrastim to increase the production of white blood cells, and rifaximin, ademetionine, ursodeoxycholic acid, glutathione for liver dysfunction along with other supportive medications was given. The patient improved clinically over 10 days and became afebrile with stabilized liver parameters. Repeat blood culture was sterile on the 12th day. He was discharged with the advice to continue oral Trimethoprim/Sulfamethoxazole combination for 6 months. A monthly follow-up was also recommended to keep track of his condition since he was prone to complications.
Conclusion:
Proper diagnosis of melioidosis in a time-sensitive manner will prevent complications and reduce mortality. Well-versed clinical recognition of physical symptoms presented by the patient and laboratory diagnosis of the causative organism plays an important role in the early diagnosis of melioidosis.