Abstract
Introduction
Non-dysraphic intramedullary lipoma in children is a very rare entity. Patients may only exhibit partial recovery after surgical intervention/debulking/excision due to the challenging intramedullary location. An unusual case of extensive intramedullary lipoma of the cervicothoracic spinal cord causing spinal compression is described. We made a revision of the literature and reported the clinical presentation as well as treatment options for this disease.
Case Presentation
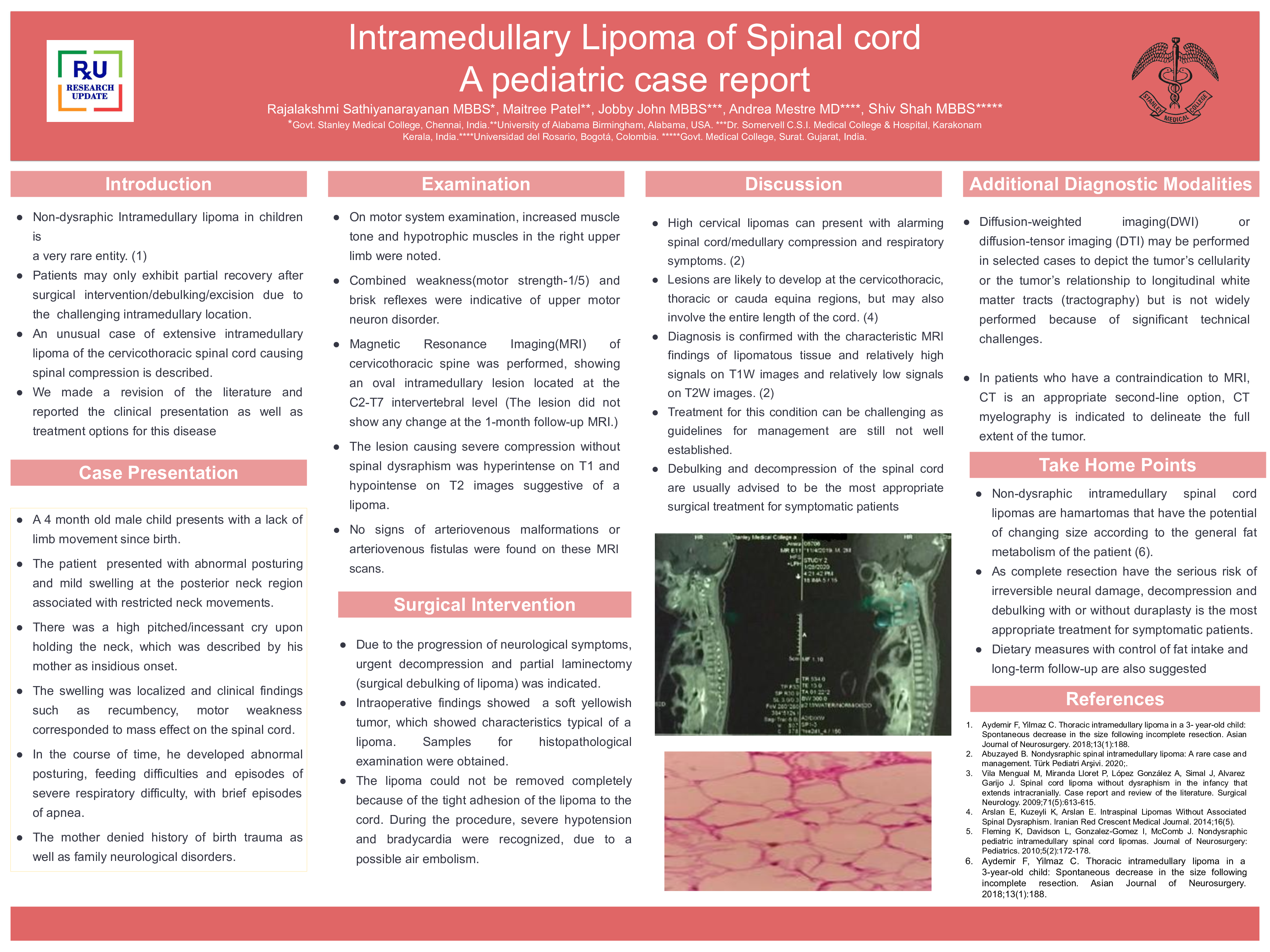
We present a case of a 4 month old male child with intramedullary lipoma in the cervico - thoracic region and lack of limb movement since birth, the cause of which remained obscure. In the course of time, he developed abnormal posturing, feeding difficulties and episodes of severe respiratory difficulty, with brief periods of apnea. The mother denied a history of birth trauma as well as family neurological disorders. On motor system examination, increased muscle tone and hypotrophic muscles in the right upper limb were noted. Combined weakness (motor strength-1/5) and brisk reflexes were indicative of upper motor neuron disorder. Magnetic Resonance Imaging (MRI) of cervicothoracic spine was performed, showing an oval intramedullary lesion located at the C2-T7 intervertebral level (The lesion did not show any change at the 1-month follow-up MRI) diagnostic for intramedullary lipoma. Urgent decompression and partial laminectomy (surgical debulking of lipoma) was performed. Intraoperative findings showed a soft yellowish tumor, which showed characteristics typical of a lipoma. Samples for histopathological examination were obtained. The lipoma could not be removed completely because of the tight adhesion to the cord. During procedure, severe hypotension and bradycardia were recognized, due to a possible air embolism.
Discussion
High cervical lipomas can present with alarming spinal cord/medullary compression and respiratory symptoms. Lesions are likely to develop at the cervicothoracic, thoracic or cauda equina regions, but may also involve the entire length of the cord. Diagnosis is confirmed with the characteristic MRI findings of lipomatous tissue and relatively high signals on T1W images and relatively low signals on T2W images. Treatment for this condition can be challenging as guidelines for management are still not well established. Debulking and decompression of the spinal cord are usually advised to be the most appropriate surgical treatment for symptomatic patients. Diffusion-weighted imaging (DWI) or diffusion-tensor imaging (DTI) may be performed in selected cases to depict the tumor’s cellularity or the tumor’s relationship to longitudinal white matter tracts (tractography) but is not widely performed because of significant technical challenges. In patients who have a contraindication to MRI, CT is an appropriate second-line option, CT myelography is indicated to delineate the full extent of the tumor.
Conclusion:
Non-dysraphic intramedullary spinal cord lipomas are hamartomas that have the potential of changing size according to the general fat metabolism of the patient. As complete resection has the serious risk of irreversible neural damage, decompression and debulking with or without duraplasty is the most appropriate treatment for symptomatic patients. Dietary measures with control of fat intake and long-term follow-up are also suggested.