Abstract
Introduction:
Pantoea agglomerans infections commonly present in patients who are immunocompromised or have in-dwelling catheters. There have been several epidemics of nosocomial septicemia with fatal cases documented in the literature. Here, we present a case of prolonged untreated P. agglomerans bacteremia with endocarditis.
Case Presentation:
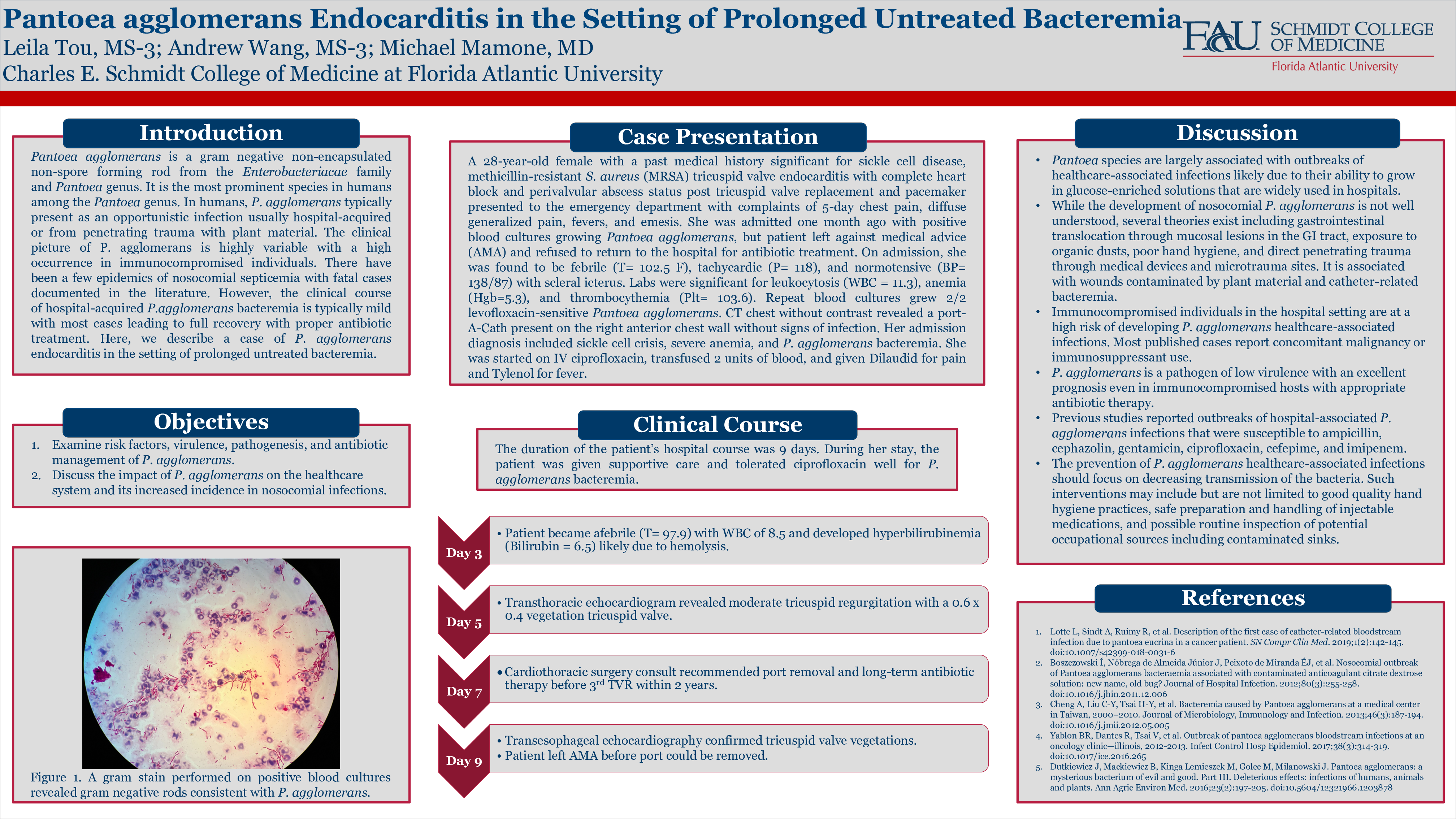
We present a 28-year-old female with a past medical history significant for sickle cell disease, methicillin-resistant Staphylococcus aureus (MRSA) tricuspid valve endocarditis with complete heart block and perivalvular abscess status-post tricuspid valve replacement and pacemaker. She presented with 5 days of chest pain, diffuse bone pain, fevers, and vomiting. During a previous hospitalization for sickle cell crisis from one month ago, her blood cultures were positive for P. agglomerans, but the patient left against medical advice before antibiotic therapy could be initiated. On physical examination, the patient was febrile and tachycardic with icteric sclera. A port-A-Cath was present on the right anterior chest wall without signs of infection. Blood cultures were repeated and grew 2/2 P. agglomerans. A vegetation on the tricuspid valve was noted on the transthoracic echocardiogram and was confirmed by a transesophageal echocardiogram. The cardiothoracic surgery consult deemed that the patient was not a candidate for valve replacement, so she was managed with IV Levaquin. On day 9 of admission, she left against medical advice.
Discussion:
Pantoea agglomerans is a rare cause of opportunistic infection most commonly hospital-acquired or from penetrating trauma with plant material. A review of the literature revealed that P. agglomerans bacteremia is frequently associated with contaminated medical equipment. There is a paucity of studies documenting cases of sporadic bacteremia associated with this pathogen. P. agglomerans bacteremia causes a diverse clinical picture and can be successfully treated with proper antibiotic use.