Abstract
Background:
The estimated incidence of cryptococcal meningitis is 200,000 new cases annually with a 1-year mortality rate of approximately 20-30% even with long-term antifungal treatment. As an opportunistic infection, cryptococcosis often presents in patients with HIV/AIDS accounting for 85% of all cryptococcal cases. Rarely, cryptococcosis can present in apparently immunocompetent patients accounting for up to 17-22% of cases in a reported series of non-HIV and non-transplant infected patients. A retrospective study revealed a substantially delayed diagnosis in immunocompetent patients (81 days) as compared to their immunocompromised counterparts (34 days). Here, we present a rare case of cryptococcal meningitis in an immunocompetent individual with no known risk factors.
Case Description:
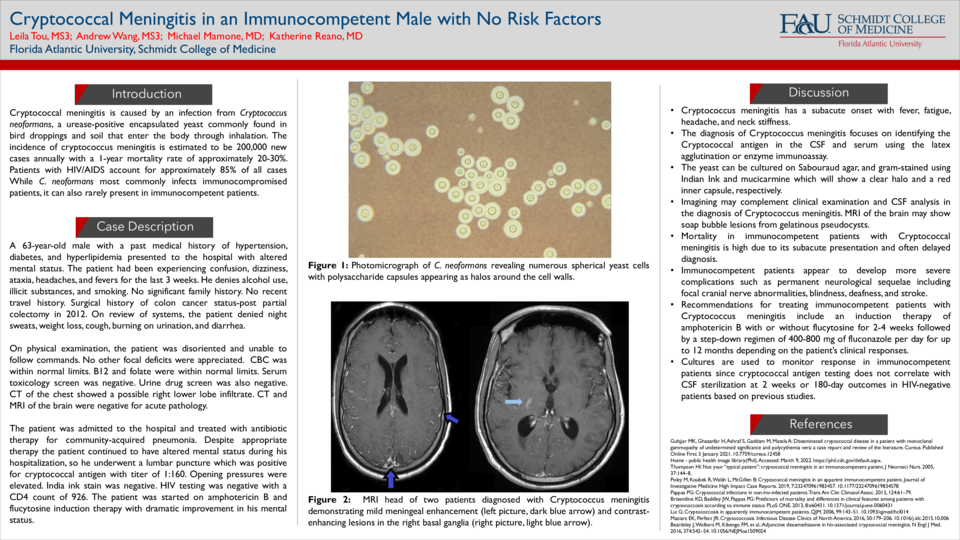
A 63-year-old male with a past medical history of hypertension, diabetes, and hyperlipidemia presented to the hospital with altered mental status. The patient had been experiencing confusion, dizziness, ataxia, headaches, and fevers for the last 3 weeks. On review of systems, the patient denied night sweats, weight loss, cough, burning on urination, and diarrhea. On physical examination, the patient was disoriented and unable to follow commands. No other focal deficits were appreciated. CBC, B12, and folate were within normal limits. CT of the chest showed a possible right lower lobe infiltrate. CT and MRI of the brain were negative. The patient was treated with antibiotic therapy for community-acquired pneumonia. Despite appropriate therapy, the patient continued to have altered mental status, so he underwent a lumbar puncture. CSF fluid was positive for cryptococcal antigen with a titer of 1:160 and elevated opening pressures. India ink stain was negative. HIV testing was negative. The patient was started on amphotericin B and flucytosine induction therapy with dramatic improvement in his mental status over the next several days.
Discussion:
This case illustrates the need to recognize cryptococcal meningitis even in immunocompetent patients especially since mortality is high due to its subacute presentation and often delayed diagnosis. Immunocompetent patients with cryptococcal meningitis develop more severe outcomes and complications such as permanent neurological sequela. A retrospective study of 302 patients diagnosed with cryptococcosis between 1996 and 2010 revealed that mortality was highest in the apparently immunocompetent group (27%). It is poorly understood why these patients fare no better or perhaps even worse than their immunocompromised counterparts. Current treatment recommendations for immunocompetent hosts with cryptococcal meningitis are based on clinical trials performed on HIV/AIDS patients or prospective studies involving HIV-negative patients. However, the duration of induction for therapy in immunocompetent patients is not well studied. For immunocompetent patients, many experts recommend an induction therapy of amphotericin B with or without flucytosine for 2-4 weeks followed by a step-down regimen of 400-800 mg of fluconazole daily for up to 12 months depending on the patient’s clinical responses. More studies and documentation of cases involving Cryptococcal meningitis in the immunocompetent population could provide critical insight into the mechanism of disease and more effective therapy.