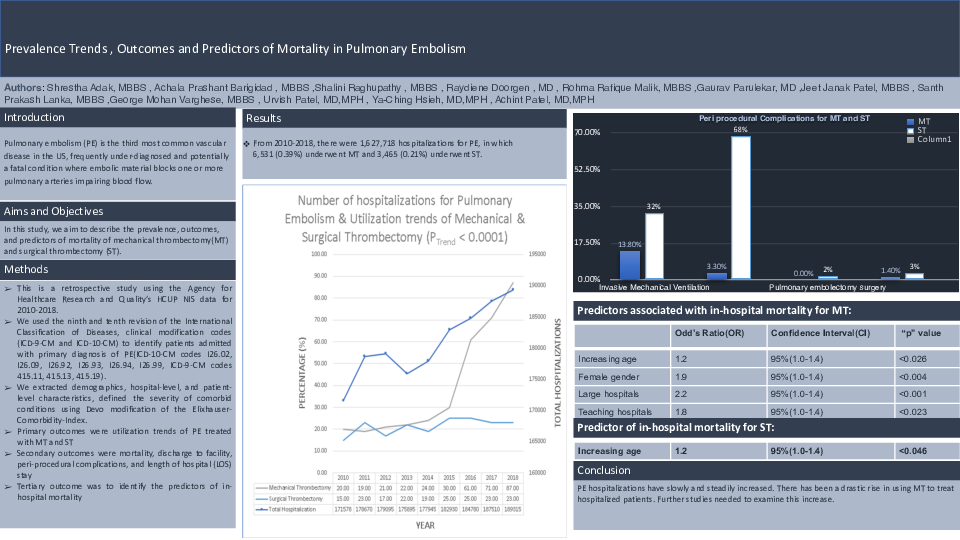
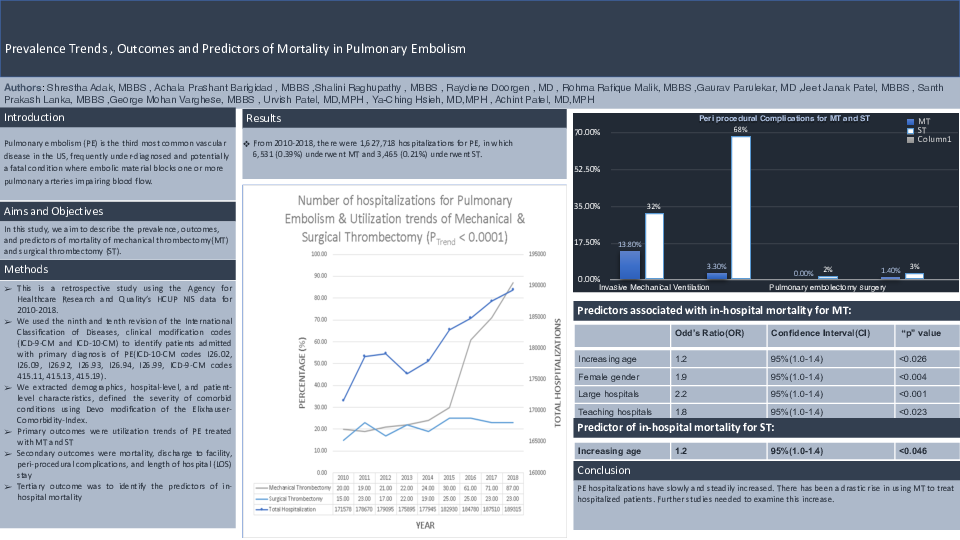
Prevalence Trends, Outcomes and Predictors of Mortality in Pulmonary Embolism
General Surgery, Medical College and Hospital, Kolkata, Kolkata, IND
Shrestha Adak, Achala Prashant Barigidad, Medical StudentMedical Student, Bangalore Medical College and research Institute, Bangalore, IND
Achala Prashant Barigidad, Shalini Raghupathy, Medical StudentMedicine and Surgery, K A P VISHWANADHAM, Tiruchirapalli, IND
Shalini Raghupathy, Raydiene Doorgen, MDMedical Student, American University of Antigua, St. John's, ATG
Raydiene Doorgen, Rohma R. Malik, Resident Physician, MDAnesthesiology, RAK Medical and Health Sciences University, Ras Al Khaimah, ARE
Rohma R. Malik, Gaurav ParulekarResearch, Icahn School of Medicine at Mount Sinai, New york city, USA
Gaurav Parulekar, Jeet J. PatelPediatrics, Boystown medical center, Omaha, USA
Jeet J. Patel, Santh Prakash Lanka , MDInternal medicine, Rangaraya Medical College, Kakinada, IND
Santh Prakash Lanka , George M. Varghese, Medical StudentMedicine and Surgery, Kasturba Medical College, Manipal, Manipal, IND
George M. Varghese, Urvish K. Patel, MD, MPHPublic Health and Neurology, Icahn School of Medicine at Mount Sinai, New York, USA
Urvish K. Patel, Ya-Ching Hsieh, MD, MPHAnesthesiology, The Icahn School of Medicine at Mount Sinai, New York, USA
Ya-Ching Hsieh, Achint A. Patel, MD, MPHIndependent Researcher, Icahn School of Medicine at Mount Sinai, Pennsylvania, USA
Achint A. Patel