Abstract
Introduction:
Herpes Simplex Virus esophagitis (HSVE) rarely presents in an immunocompetent host with acute onset of odynophagia, heartburn and fevers without ulcers. Incidence of HSVE is higher among males compared to females with a ratio of 3:1. Here we present a case of a middle-aged immunocompetent male with HSVE.
Case report:
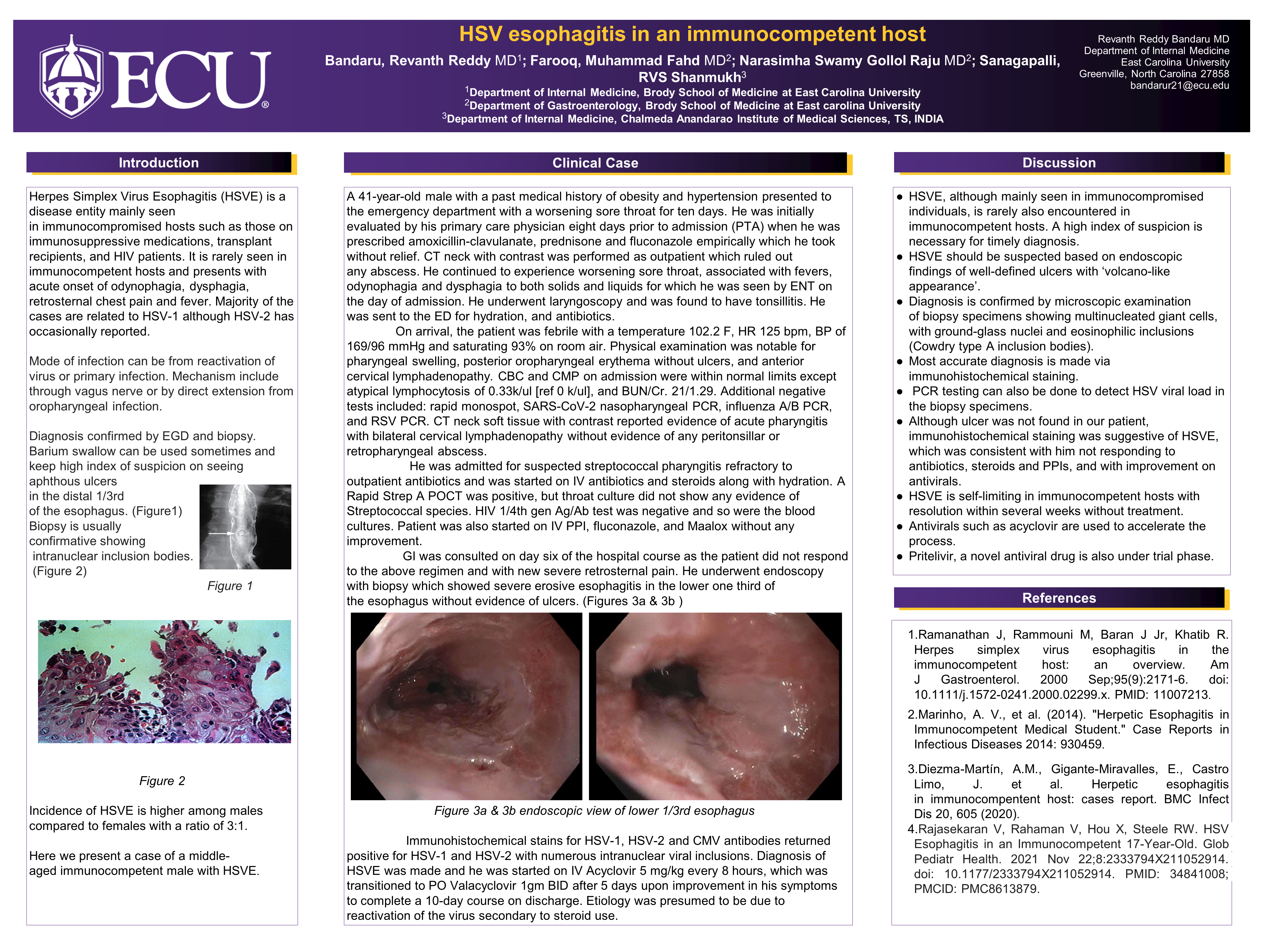
A 41-year-old male was sent by ENT to the ED with a worsening sore throat for ten days. He was initially evaluated by his PCP eight days PTA when he was prescribed amoxicillin-clavulanate, prednisone and fluconazole empirically which he took without relief. Associated symptoms included fevers, odynophagia and dysphagia to both solids and liquids for which he was seen by ENT on the day of admission and underwent laryngoscopy with findings of tonsillitis. On arrival, he was febrile and tachycardic. Physical examination was notable for posterior oropharyngeal erythema and swelling without ulcers, and anterior cervical lymphadenopathy. Labs showed evidence of atypical lymphocytosis. CT neck soft tissue neck with contrast ruled out abscess. He received Clindamycin, Penicillin, and Dexamethasone. A Rapid Strep test was positive, but throat culture was negative. He underwent endoscopy with biopsy, which showed erosive esophagitis in the lower third of the esophagus without ulcers. Immunohistochemical stains returned positive for HSV-1 and HSV-2 with numerous intranuclear viral inclusions on path. He was diagnosed with HSVE and started on IV Acyclovir, which was transitioned to PO Valacyclovir upon improvement in his symptoms to complete a 10-day course.
Discussion:
A high index of suspicion is necessary in immunocompetent hosts for timely diagnosis of HSVE. Most accurate diagnosis is made via immunohistochemical staining of biopsy specimens. In our patient, although no ulcer was found, immunohistochemical staining was suggestive of HSVE. This was consistent with his improvement on antivirals.