Abstract
Introduction: Despite the excellent and effective action profile, rare cardiovascular events have been encountered with Liposomal amphotericin B usage. Though sporadic adverse events have emerged before, the interplay between this drug and the novel coronavirus remains a mystery.
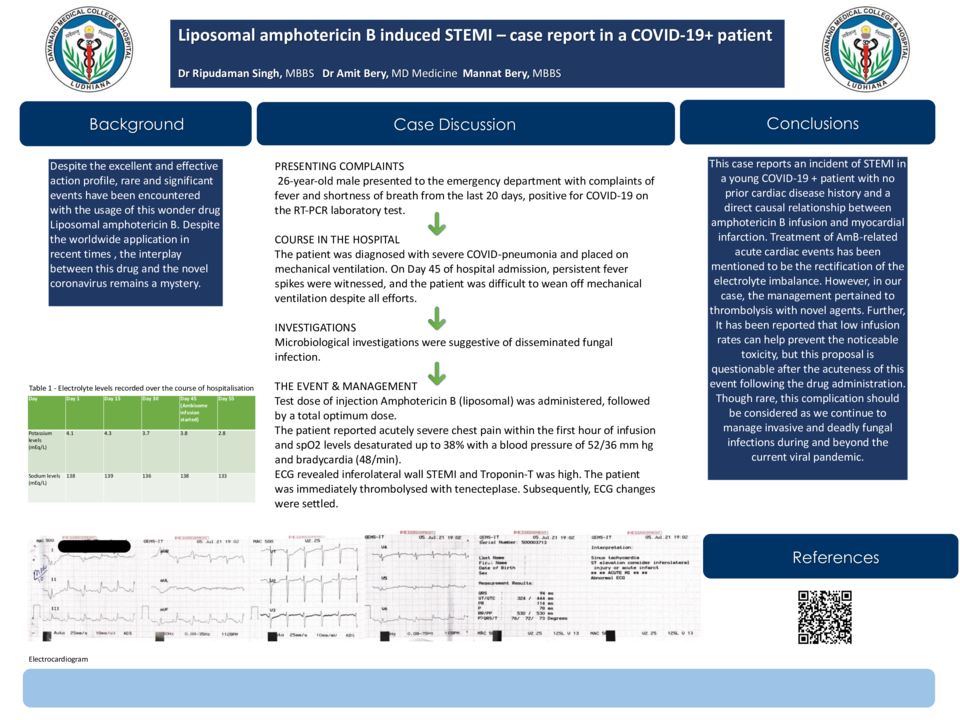
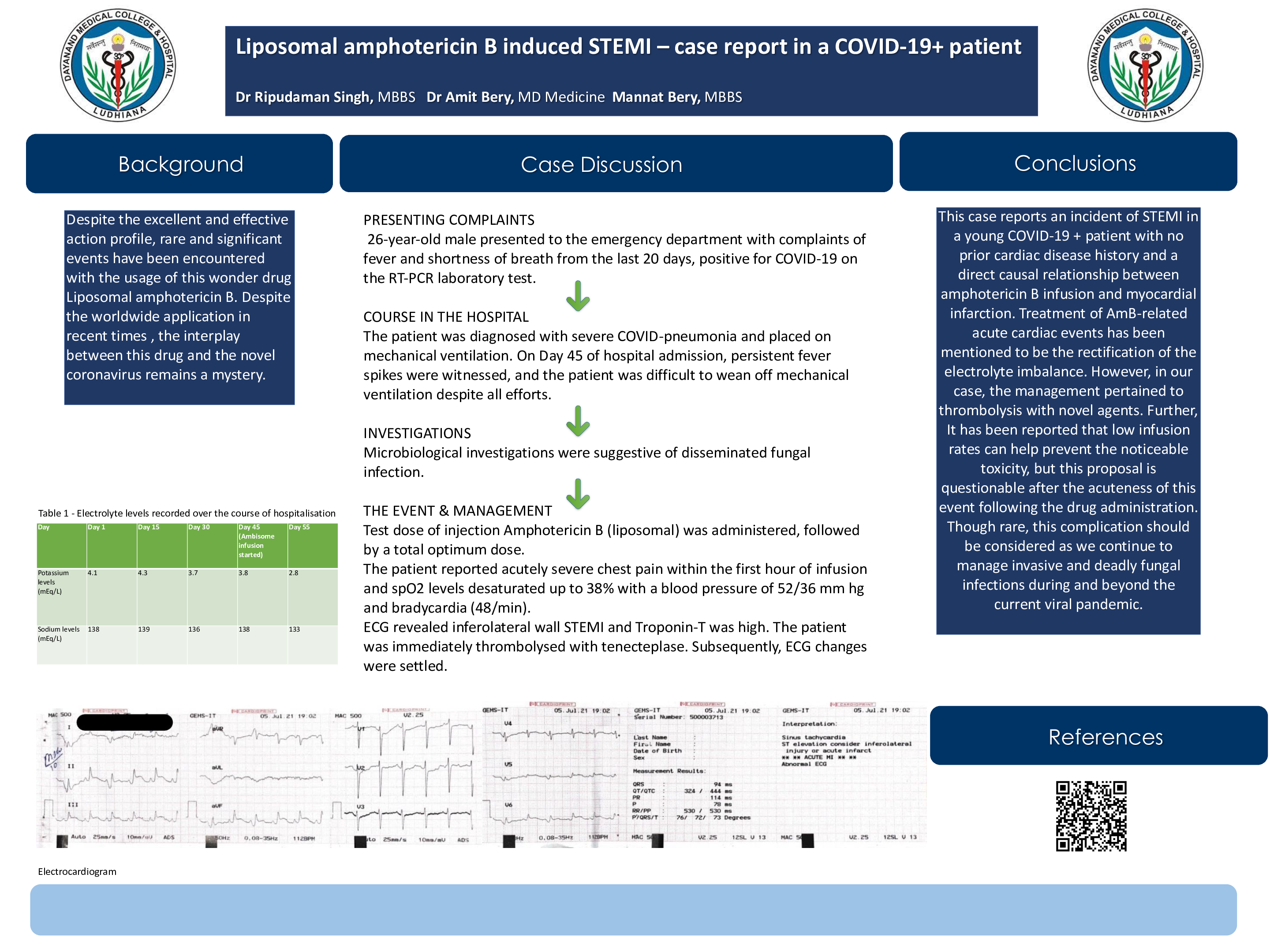
Case description: A 26-year-old male presented to the emergency department with complaints of fever and shortness of breath from the last 20 days, positive for COVID-19 on the RT-PCR laboratory test. The patient was diagnosed with severe COVID-pneumonia and placed on mechanical ventilation. On Day 45 of hospital admission, persistent fever spikes were witnessed, and the patient was difficult to wean off mechanical ventilation despite all efforts. Microbiological investigations were suggestive of disseminated fungal infection. A test dose of injection Amphotericin B (liposomal) was administered, followed by a total optimum dose. The patient reported acutely severe chest pain within the first hour of infusion and spO2 levels desaturated up to 38% with a blood pressure of 52/36 mm hg and bradycardia (48/min). ECG revealed inferolateral wall STEMI and Troponin-T was high. The patient was immediately thrombolysed with tenecteplase. Subsequently, ECG changes were settled.
Discussion: This case reports an incident of STEMI in a young COVID-19 + patient with no prior cardiac disease history and a direct causal relationship between amphotericin B infusion and myocardial infarction. Treatment of AmB-related acute cardiac events has been mentioned to be the rectification of the electrolyte imbalance. However, in our case, the management pertained to thrombolysis with novel agents. Further, It has been reported that low infusion rates can help prevent the noticeable toxicity, but this proposal is questionable after the acuteness of this event following the drug administration. Though rare, this complication should be considered as we continue to manage invasive and deadly fungal infections during and beyond the current viral pandemic.