Abstract
Objectives: To date, the role of SRS without whole brain irradiation (RT) is a well-recognized treatment option for patients with limited intracranial disease (1-4 BMs) and a life-expectancy of more than 3-6 months. However, recent data show that this treatment approach can be preferred also for patients with multiple BMs. Modern RT techniques applied to Linac-based SRS, including flattening filter free volumetric modulated arc therapy (VMAT), have increased the precision of treatment, improving target dose distribution and reducing normal tissue doses. In this context, a new dedicated mono-isocenter technique with multiple non-coplanar arcs could be performed, allowing to minimize overall treatment time (OTT) and geometrical/setup uncertainties. Here, we compare 2 different optimization approaches in terms of isodose prescription, target coverage and organs at risk (OARs)dose sparing.
Methods: From August to October 2019, 69 BMs (mean7, range4–21) have been treated by Single iscocenter SRS in 10 patients. The prescribed dose (Dp) was 27Gy in 3 fractions. Planning Target Volume (PTV) was defined by 1 mm isotropic margin from each lesion. None of PTVs was overlooking to chiasm or brainstem. Mono-isocenter VMAT plans with 5 non-coplanar arcs (couch at 0°, ±45°, ±90°) were generated for all patients, while 2 different modalities of optimization – one based on mono-isocenter SRS dedicated optimization tool and the other on human experience – were compared: ALDO vs ILA. A dose normalization of 100%Dp at 98%PTV was adopted, while D2%(PTV)<150%Dp was accepted. OARs were defined as chiasm, brainstem and heathy brain minus PTVs. Plan-optimizations were compared by the isodose prescription, D100% and D2% for PTVs, maximum dose for chiasm and brainstem, V18Gy for the healthy brain, number of monitor units (MU) and OTT.
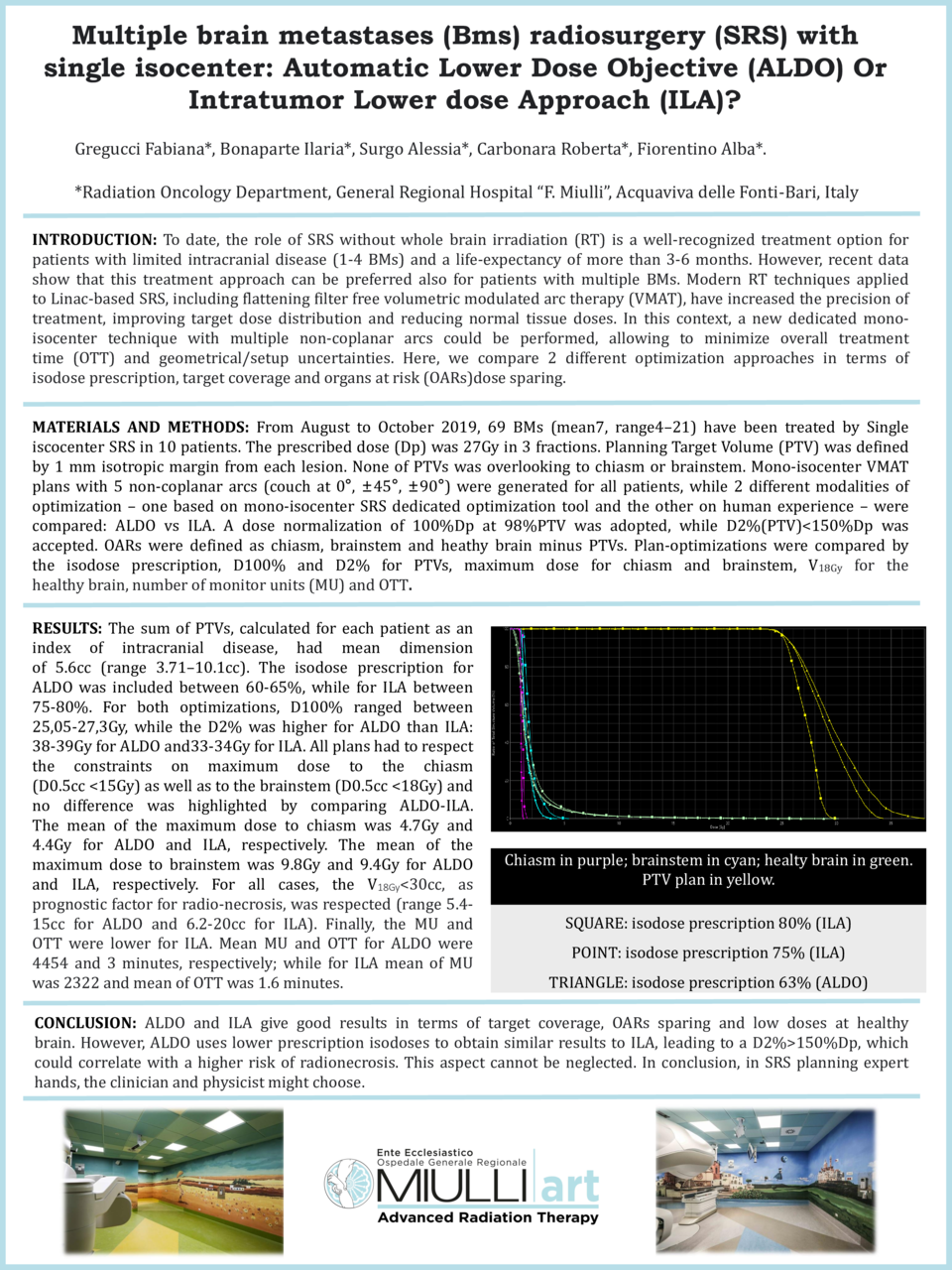
Results: The sum of PTVs, calculated for each patient as an index of intracranial disease, had mean dimension of 5.6cc (range 3.71–10.1cc). The isodose prescription for ALDO was included between 60-65%, while for ILA between 75-80%. For both optimizations, D100% ranged between 25,05-27,3Gy, while the D2% was higher for ALDO than ILA: 38-39Gy for ALDO and33-34Gy for ILA. All plans had to respect the constraints on maximum dose to the chiasm (D0.5cc <15Gy) as well as to the brainstem (D0.5cc <18Gy) and no difference was highlighted by comparing ALDO-ILA. The mean of the maximum dose to chiasm was 4.7Gy and 4.4Gy for ALDO and ILA, respectively. The mean of the maximum dose to brainstem was 9.8Gy and 9.4Gy for ALDO and ILA, respectively. For all cases, the V18Gy<30cc, as prognostic factor for radio-necrosis, was respected (range 5.4-15cc for ALDO and 6.2-20cc for ILA). Finally, the MU and OTT were lower for ILA. Mean MU and OTT for ALDO were 4454 and 3 minutes, respectively; while for ILA mean of MU was 2322 and mean of OTT was 1.6 minutes.
Conclusion: ALDO and ILA give good results in terms of target coverage, OARs sparing and low doses at healthy brain. However, ALDO uses lower prescription isodoses to obtain similar results to ILA, leading to a D2%>150%Dp, which could correlate with a higher risk of radionecrosis. This aspect cannot be neglected. In conclusion, in SRS planning expert hands, the clinician and physicist might choose between ALDO or ILA to customize treatments based on histology, BMs size and number, proximity to OARs, performing treatment plan optimization tailored on the patient.