Abstract
The two options often considered for treatment of brain metastases are a course of noninvasive radiation therapy with Stereotactic Radiosurgery (SRS) or a safe gross total resection followed by radiation therapy to the surgical resection cavity (Post-Op). After consideration of many factors (size, location, number of lesions, histology, etc.), the latter treatment course is often chosen. In principle, this Post-Op course of treatment enhances the therapeutic ratio by reducing the required tumor volume and, thereby, improving the efficacy of the treatment. Though the principle seems sound, this resection-benefit in terms of treatment parameters and tissues of the normal brain remains to be validated. Our study aims to retrospectively compare the plan parameters of SRS plans delivered to intact brain metastases and plans delivered to the tumor beds from which the brain metastases were resected.
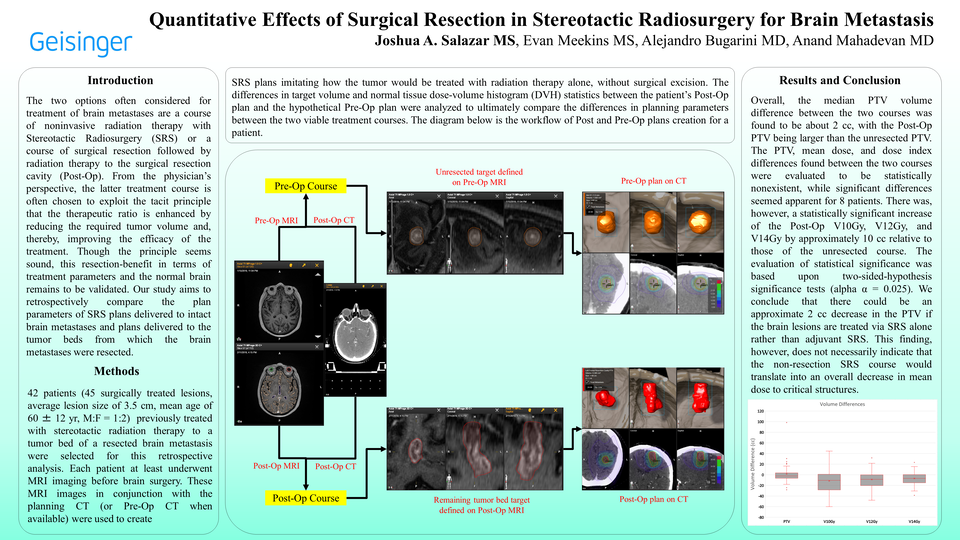
42 patients (45 surgically treated lesions, average lesion size of 3.5 cm, mean age of 60 ± 12 yr, M:F = 1:2) previously treated with stereotactic radiation therapy to the tumor bed were selected for this retrospective analysis. Each patient underwent volumetric imaging prior to surgical intervention. These images were used to create SRS plans imitating how the tumor would be treated with radiation therapy alone, without surgical excision. The target volume and normal tissue dose-volume histogram (DVH) planning parameters for both the Post-Op and the hypothetical non-resection radiation treatment course were analyzed and compared.
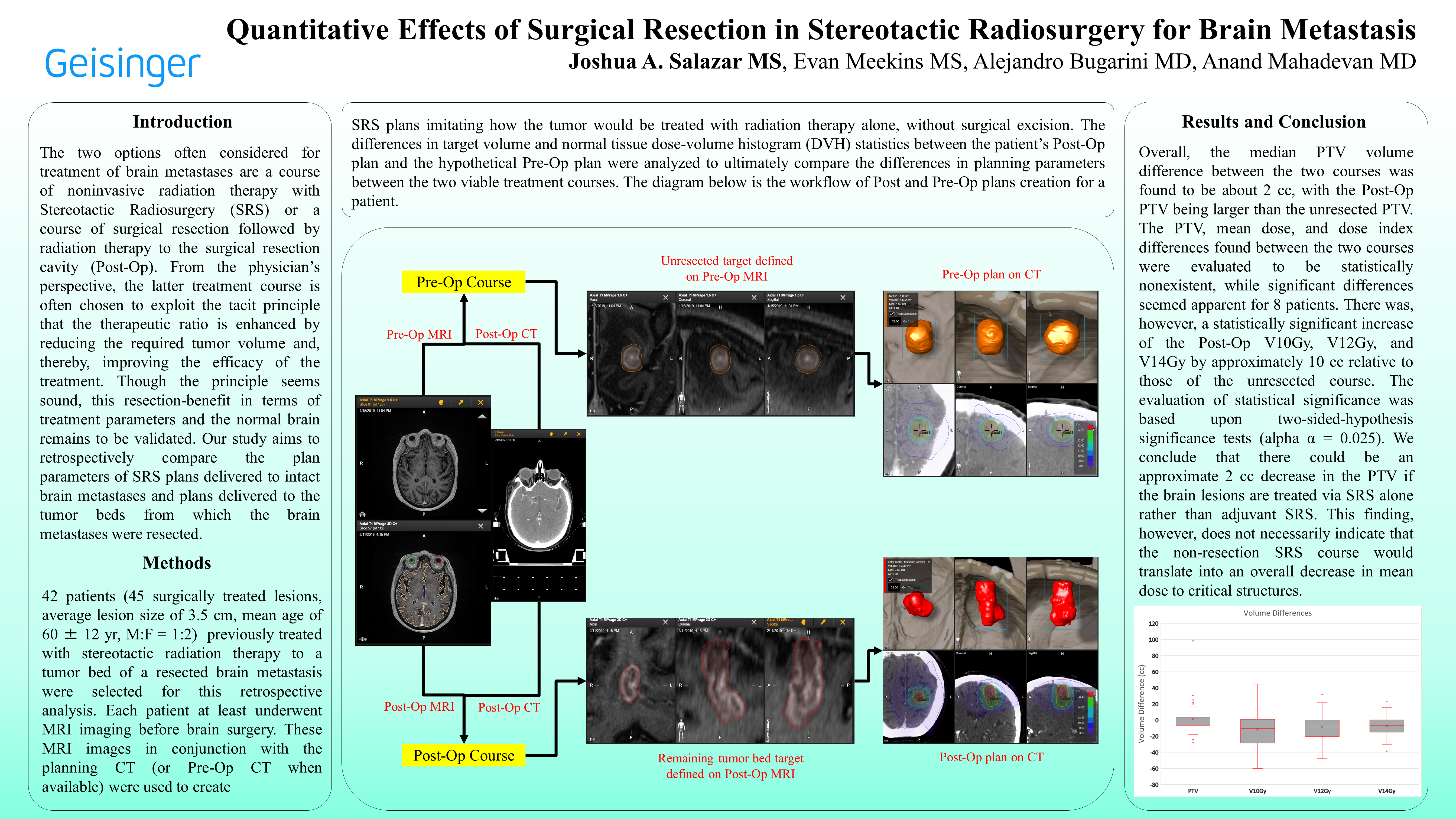
Comparisons of DVH statistics and Planning Target Volume (PTV) size between the two viable courses did not show decreases in Post-Op PTV, mean normal tissue doses nor discrepancies in dose indexes. Overall, the median PTV difference between the two courses was found to be about 2 cc, with the Post-Op PTV being larger than the unresected PTV. Furthermore, the differences between mean doses to critical structures (brainstem, optic chiasm, hippocampi) and dose indexes (Conformity and Gradient index) were found to be negligible for the overall cohort but significant for 8 individual patients (whom had at least one DVH statistic value two times that of the respective DVH standard deviation); These individual patients seemed to have structures receiving larger mean dose or plans with larger dose indexes in either the unresected or Post-Op treatment based on the location of their tumors. The PTV, mean dose, and dose index differences found between the two courses were evaluated to be statistically nonexistent by two-sided-hypothesis significance tests (alpha α = 0.025). The Post-Op V10Gy, V12Gy, and V14Gy increased by approximately 10 cc relative to those of the unresected course and were evaluated to be statistically significant (alpha α = 0.025).
Our study suggests there would be an approximate 2 cc decrease in PTV if the brain lesions had been treated via SRS alone rather than with adjuvant SRS, though the non-resection SRS course would not necessarily translate into an overall decrease in mean dose to critical structures because the doses to these structures were insignificant. While these specific findings lack statistical authority at this time, other findings of this study suggest a statistically significant decrease of the V10Gy, V12Gy, and V14Gy in the non-resection SRS course relative to those of the Post-Op course.