Abstract
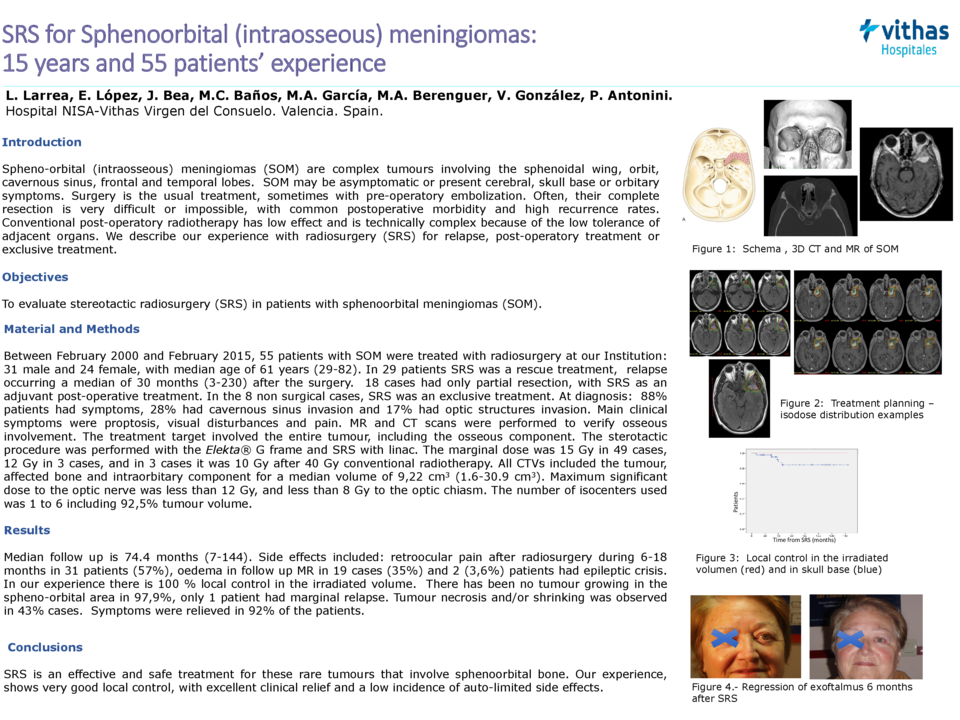
Introduction: Spheno-orbital (intraosseous) meningiomas (SOM) are complex tumours involving the sphenoidal wing, orbit, cavernous sinus, frontal and temporal lobes. SOM may be asymptomatic or present cerebral, skull base or orbitary symptoms. Surgery is the usual treatment, sometimes with pre-operatory embolization. Often, their complete resection is very difficult or impossible, with common postoperative morbidity and high recurrence rates. Conventional post-operatory radiotherapy has low effect and is technically complex because of the low tolerance of adjacent organs. We describe our experience with radiosurgery (SRS) for relapse, post-operatory treatment or exclusive treatment.
Objectives: To evaluate stereotactic radiosurgery (SRS) in patients with sphenoorbital meningiomas (SOM).
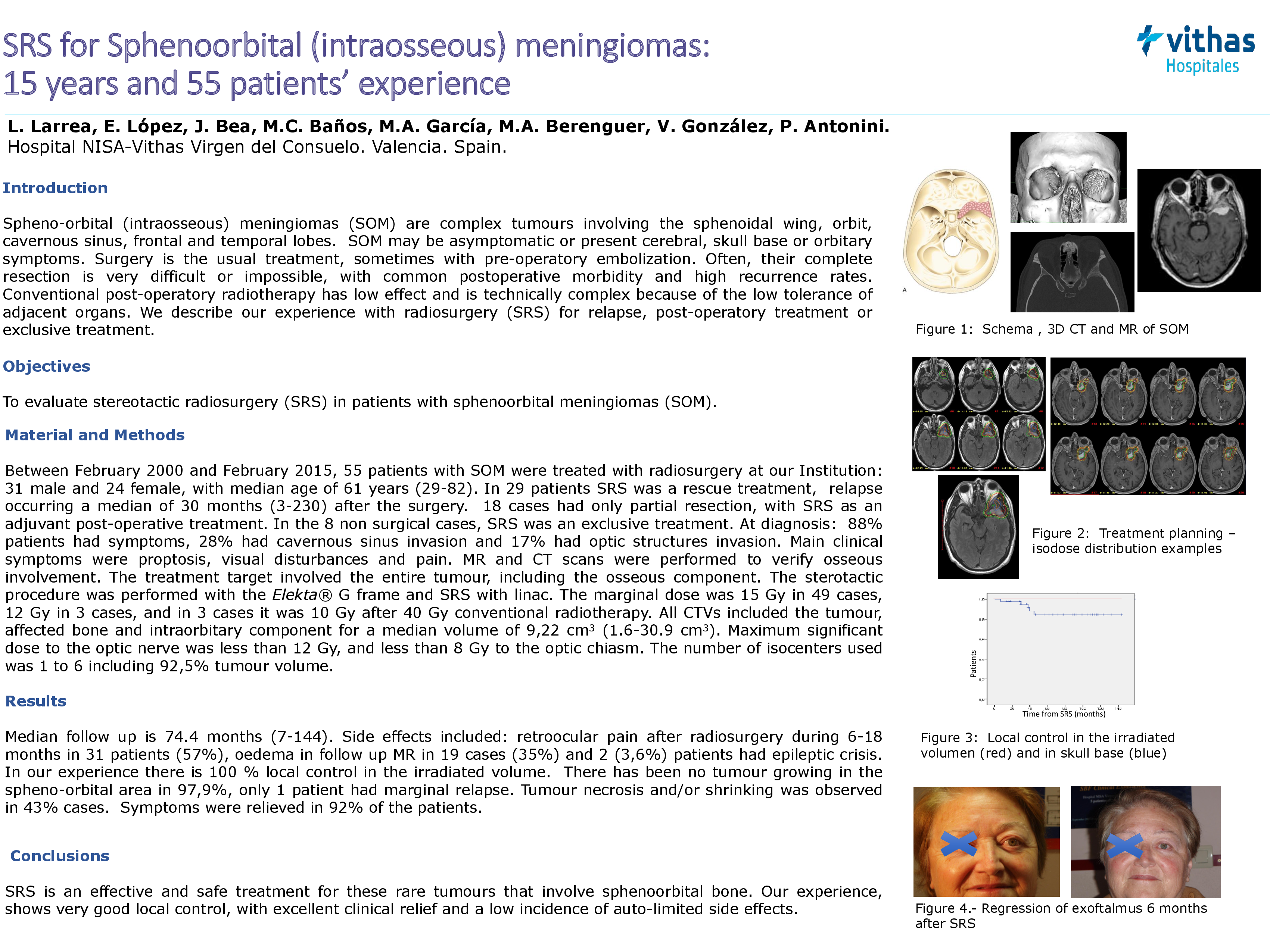
Methods: Between February 2000 and February 2015, 55 patients with SOM were treated with radiosurgery at our Institution: 31 male and 24 female, with median age of 61 years (29-82). In 29 patients SRS was a rescue treatment, relapse occurring a median of 30 months (3-230) after the surgery. 18 cases had only partial resection, with SRS as an adjuvant post-operative treatment. In the 8 non surgical cases, SRS was an exclusive treatment. At diagnosis: 88% patients had symptoms, 28% had cavernous sinus invasion and 17% had optic structures invasion. Main clinical symptoms were proptosis, visual disturbances and pain. MR and CT scans were performed to verify osseous involvement. The treatment target involved the entire tumour, including the osseous component. The sterotactic procedure was performed with the Elekta® G frame and SRS with linac. The marginal dose was 15 Gy in 49 cases, 12 Gy in 3 cases, and in 3 cases it was 10 Gy after 40 Gy conventional radiotherapy. All CTVs included the tumour, affected bone and intraorbitary component for a median volume of 9,22 cm3 (1.6-30.9 cm3). Maximum significant dose to the optic nerve was less than 12 Gy, and less than 8 Gy to the optic chiasm. The number of isocenters used was 1 to 6 including 92,5% tumour volume.
Results: Median follow up is 74.4 months (7-144). Side effects included: retroocular pain after radiosurgery during 6-18 months in 31 patients (57%), oedema in follow up MR in 19 cases (35%) and 2 (3,6%) patients had epileptic crisis. In our experience there is 100 % local control in the irradiated volume. There has been no tumour growing in the spheno-orbital area in 97,9%, only 1 patient had marginal relapse. Tumour necrosis and/or shrinking was observed in 43% cases. Symptoms were relieved in 92% of the patients.
Conclusions: SRS is an effective and safe treatment for these rare tumours that involve sphenoorbital bone. Our experience, shows very good local control, with excellent clinical relief and a low incidence of auto-limited side effects.