Abstract
Purpose
The availability of image guidance and intensity modulation has led to the increasing use of hypofractionated stereotactic radiotherapy (hSRT) as an alternative to conventionally fractionated radiotherapy or radiosurgery for intracranial meningioma (ICM). As the safety and efficacy of this approach is not well characterized, we conducted a systematic review of the literature to assess the clinical outcomes of hSRT in the setting of ICM.
Methods
A systematic review of Medline and EMBASE databases was performed following the PRISMA guidelines. Included studies were retrospective or prospective series that 1) examined an ICM population of ≥ 10 patients, 2) delivered >1 fraction of photon hSRT (≥ 2.5 Gy per fraction), 3) used a LINAC-based platform, Cyberknife (CK) or multisession Gammaknife, 4) reported on clinical outcomes, and 5) had a median follow-up of ≥ 2 years. Descriptive statistics were generated for included studies.
Results
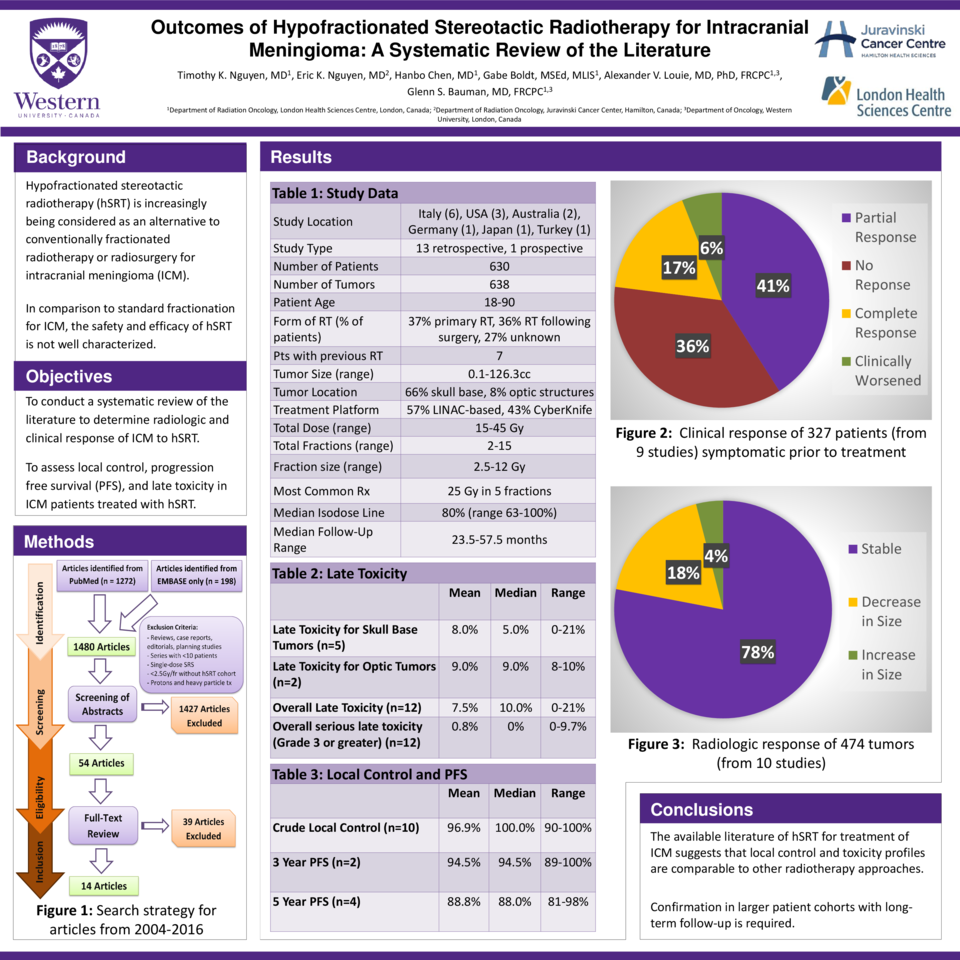
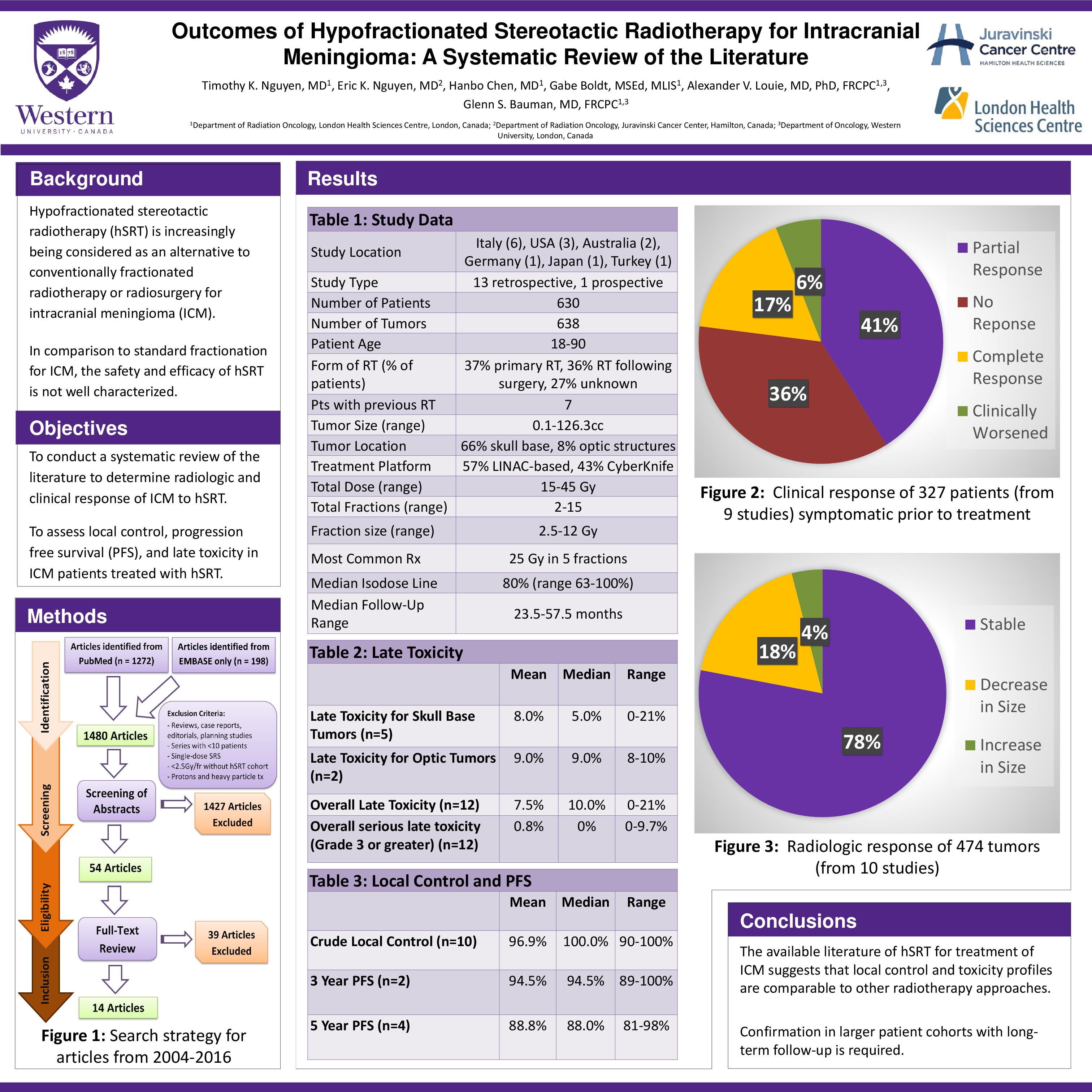
1480 initial studies, 14 met eligibility criteria for inclusion, reporting on 630 patients (age range 18-90) treated for 638 tumors. Primary RT was delivered in 37% of patients, 36% had radiation following surgery, and surgical details were unavailable in 27%. Of all tumors, 66% were located in the skull base and 8% involving optic structures. Treatment platforms included LINAC-based hSRT (57%) or CK (43%). Total dose ranged from 15-45Gy in 2-15 fractions and was prescribed to a median isodose line of 80%. The most common fractionation reported was 25/5. In 474 tumors assessed for radiologic response (median follow-up = 24.5-57.5 months), 78% remained stable, 18% decreased in size and 4% increased in size. Of 327 patients who were symptomatic prior to treatment, 17% had complete resolution, 41% had improvement, 36% had stability and 6% had deterioration post treatment. Crude local control (LC) was 90-100% as reported in 10 studies. Overall, the median late toxicity rate was 10% (range=0-21%). The median late toxicity rates for tumors involving the skull base and optic structures were 5% (range=0-21%) and 9% (range=8-10%) respectively. Most common significant late toxicities were new decrease in vision (n=8) and new cranial neuropathy (n=11).
Conclusions
While the available literature of hSRT for treatment of ICM suggests that local control and toxicity profiles are comparable to other radiotherapy approaches, confirmation in larger patient cohorts with longer follow-up is required.