Abstract
Abstract Body: Effective positive pressure ventilation is the single most important step in neonatal resuscitation. Neonatal Resuscitation Program (NRP) supports the use of the laryngeal mask airway (LMA) as an alternate airway device when endotracheal intubation is technically challenging (e.g. unsuccessful attempts, airway anomalies, or operator inexperience) (1). Practicing neonatologists have limited experience using an LMA. Proficiency is attained only after 5-24 attempts (2-4) - challenging for any practicing neonatologist. Simulation-based training that allows repeated practice and feedback may bridge this gap. Our long term aim is to develop an educational toolkit and checklist for LMA placement. Our specific aim was to perform a task analysis to identify key steps of LMA insertion as an objective method of developing a checklist for teaching and assessing this procedure.
Methods: Literature review revealed one published checklist with insufficient detail to effectively teach LMA insertion (5). A task analysis was performed to objectively detail each step and determine essential actions, optional actions, and decision points. 3 pediatric anesthesiologists (experts) performed LMA insertion on a neonatal task trainer while being videotaped. 5 neonatologists, inexperienced in neonatal LMA insertion, independently reviewed these recordings and the NRP LMA procedural video (1). Independently each developed a script that outlined the steps of LMA insertion which were de-identified and collated. A modified Delphi process was then used to create the checklist. Differences in step sequence and level of detail were resolved by consensus until complete agreement was reached.
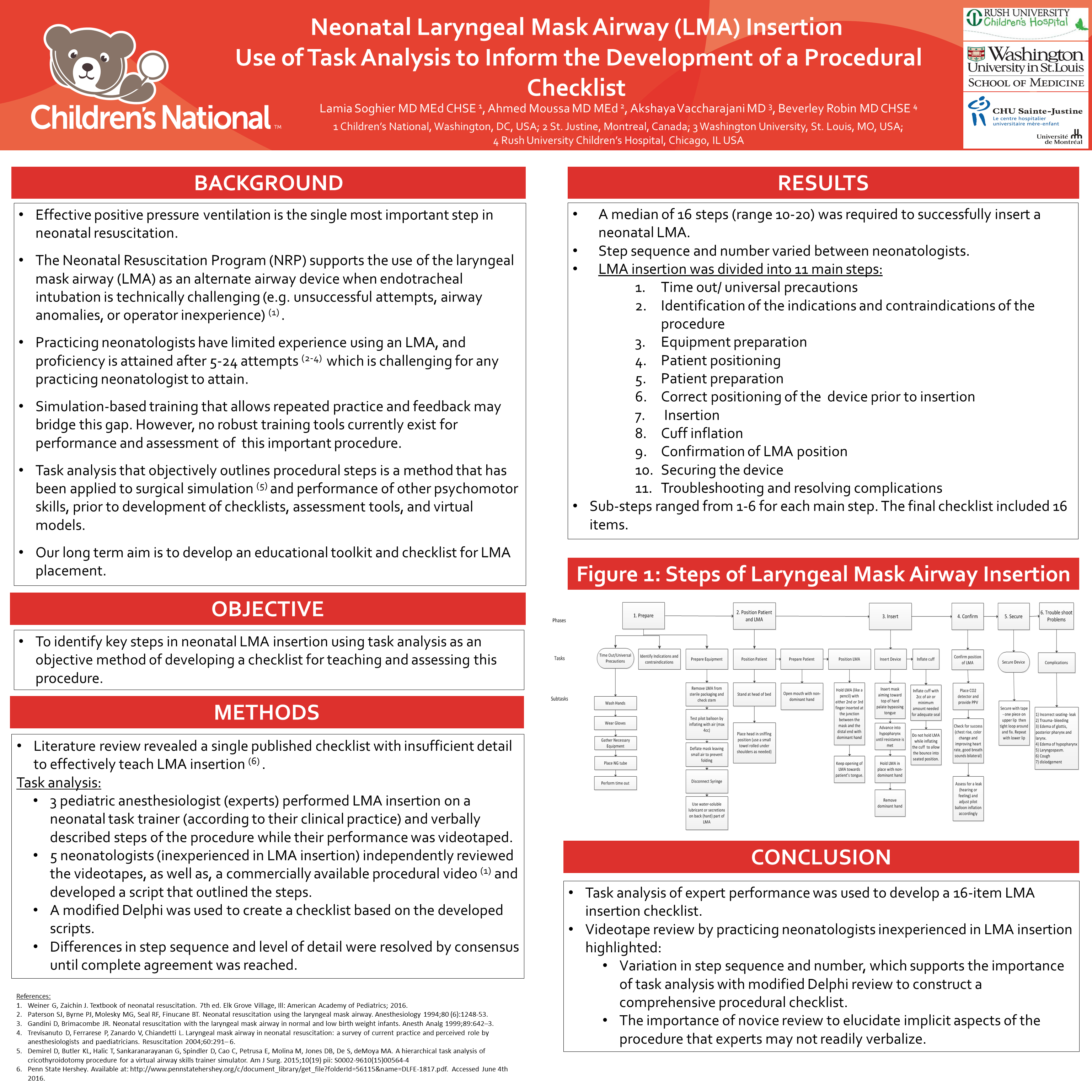
Results : Independent review of the videotapes by the 5 neonatologists revealed a median of 16 steps (range 10-20). Step sequence and level of detail varied between neonatologists. Modified Delphi and consensus review revealed 11 main steps, each with a set of associated sub-steps. The main steps include: time out/universal precautions, identification of the indications and contraindications, equipment preparation, patient positioning, patient preparation, correct positioning of the device prior to insertion, insertion, inflation of the cuff, confirmation of device position, securing the device , troubleshooting and resolving complications. Sub-steps ranged from 1-6 for each main step. The final checklist included 16 items.
Conclusion : An LMA insertion checklist was developed using task analysis. Review by inexperienced practicing neonatologists highlighted variation in step sequence, detail level and the importance of novice review to elucidate implicit aspects of the procedure that experts may not readily verbalize. We recommend performing a detailed task analysis, a method that has been applied to surgical simulation (6), prior to development of procedural checklists. Next steps include cognitive task analysis to determine the most likely technical errors that occur during LMA insertion.