Abstract
Context: Newborn care providers are required to have active Neonatal Resuscitation Program (NRP) status. NRP has specific recommendations for the structure, content and teaching methodology of its courses. NRP integrated simulation into courses in 2010. At that time instructors were required to complete a static non-mentored education on simulation. In 2015, a requirement was added for new instructors to run 2 mentored courses and receive feedback on debriefing. Given the expertise needed to run effective simulation based courses, there was concern that our Children's Hospital of Philadelphia Newborn Care Network (CNBCN) hospitals might not be meeting the recommendations from NRP and the needs of learners. The use of rigorous quality improvement (QI) methodology has allowed for large improvements in clinical care delivery. The decision was made to take a QI approach to identify gaps in the delivery of NRP courses and to develop improvement interventions. Underlying this project was the belief that by optimizing NRP courses, learners would be better prepared to deliver care in the clinical environment.
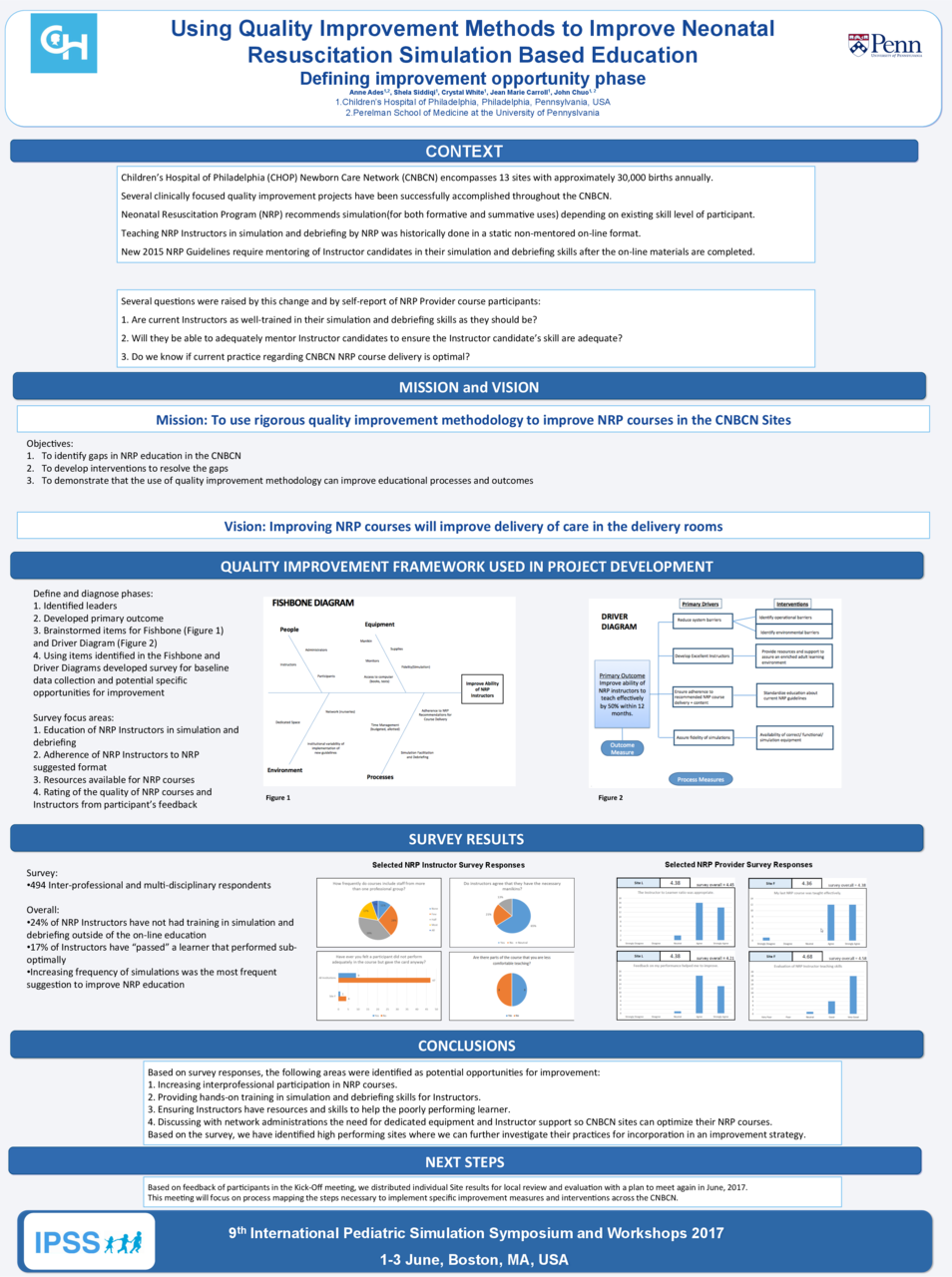
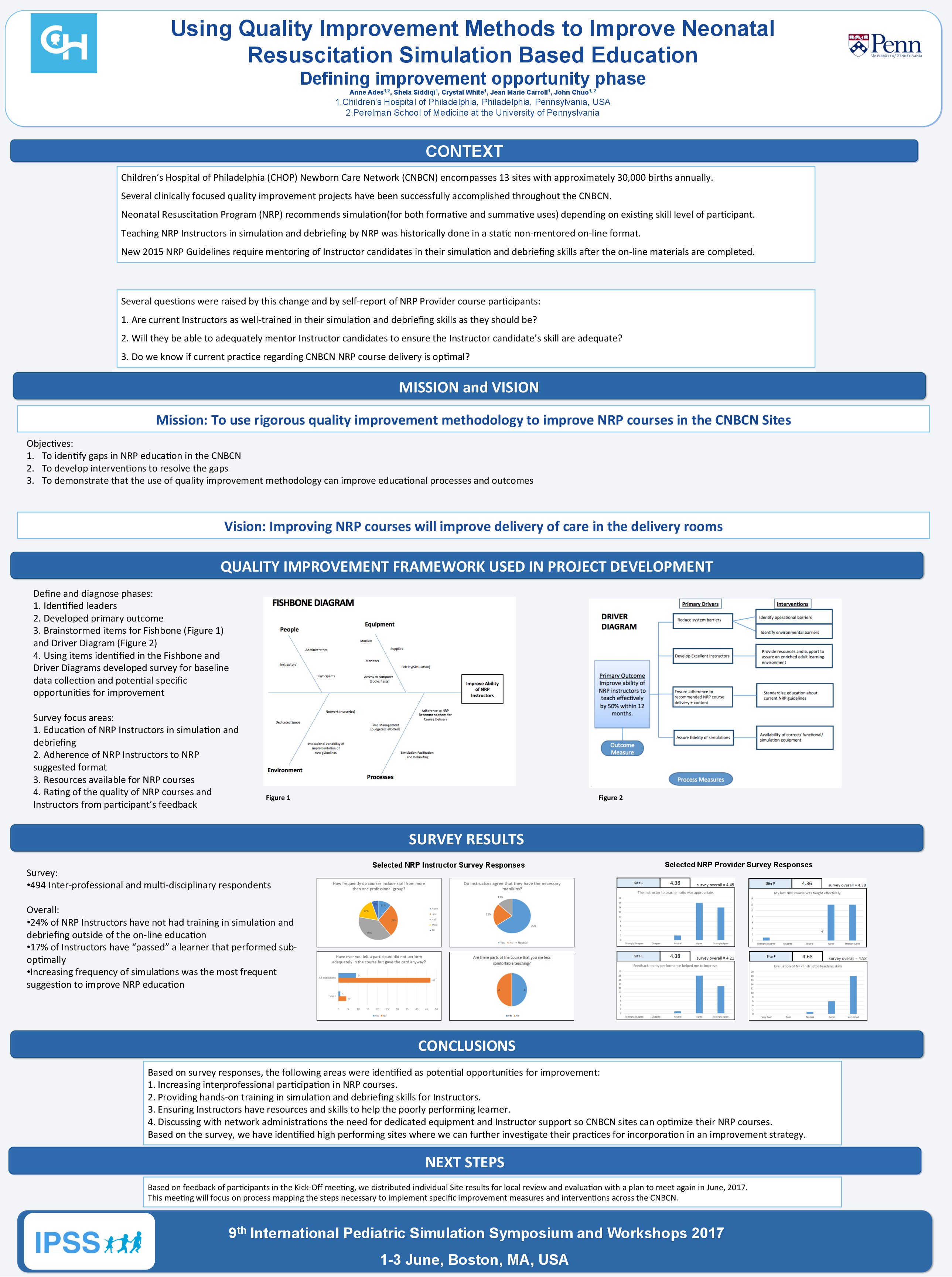
Description: CNBCN encompasses 13 sites. The project started with a primary outcome of: "Improve the ability of NRP instrucutors to teach effectively by 50% within 12 months." Fishbone and Driver diagrams were developed and utilized to support the building of a survey. The survey was designed to provide baseline data on the existing delivery of NRP education as well as identify specific areas to target for this QI initiative. A large focus of this survey centered on: 1) the education of instructors in simulation facilitation and debriefing; 2) the availability of resources; and 3) feedback from providers on the quality of their NRP instructors;
Observation/Evaluation: The survey was distributed to all CNBCN sites as well as to all providers who were responsible for caring for newborns in the delivery room. Survey respondents totaled 450. Survey responses provided the following feedback: 1) NRP instructors responded that only 78% of NRP courses were inter-professional; 2) 24% of instructors did not have any training in simulation facilitation and debriefing; 3) 17% of instructors have "passed" a student who they felt did not perform adequately; 4) providers only rated 63% of their instructors as being very good in their teaching skills; 5) only 52% of sites do simulation outside of NRP courses and 6) doing more frequent simulations was the most frequent suggestion by survey respondents for improving NRP education.
Discussion: Several areas were identified for focusing initiatives to help improve NRP instructor efficacy and ideally learner outcomes. The next step is to engage a larger workgroup of NRP stakeholders at each site to address these improvement opportunities using the IHI Model for Improvement framework, and where applicable, LEAN principles. This is a novel use of QI methodology to improve a simulation based educational program.