Abstract
Context: The Neonatal Resuscitation Program (NRP) teaches the concepts of neonatal resuscitation without necessarily training for competency. The newest 7th edition of NRP required changes to our curriculum to update to the current guidelines. We took the opportunity to examine closely our goals for each skill station and how it might be better taught. Skills were taught by NRP instructors to each class one at a time. Learners would wander around the center and look for “open” stations. Multi-disciplinary teams were not formed until later for simulations, and the teaching from instructors was quite variable in content and scope they taught at each station.
Description: We set out to standardize the teaching portion of the skills by creating videos that taught and demonstrated the skills. Skills videos cover 1) Preparation, initial steps and PPV, 2) Alternate Airway and chest compressions, and 3) Emergency UVC placement and IV epinephrine. This decreased our number of skills stations from 4 to 3 since the skills were re-organized to more realistically reflect the flow and order a neonatal resuscitation should take. Learners will be divided into multi-disciplinary groups before technical skills training to better promote behavioral skills training within teams.
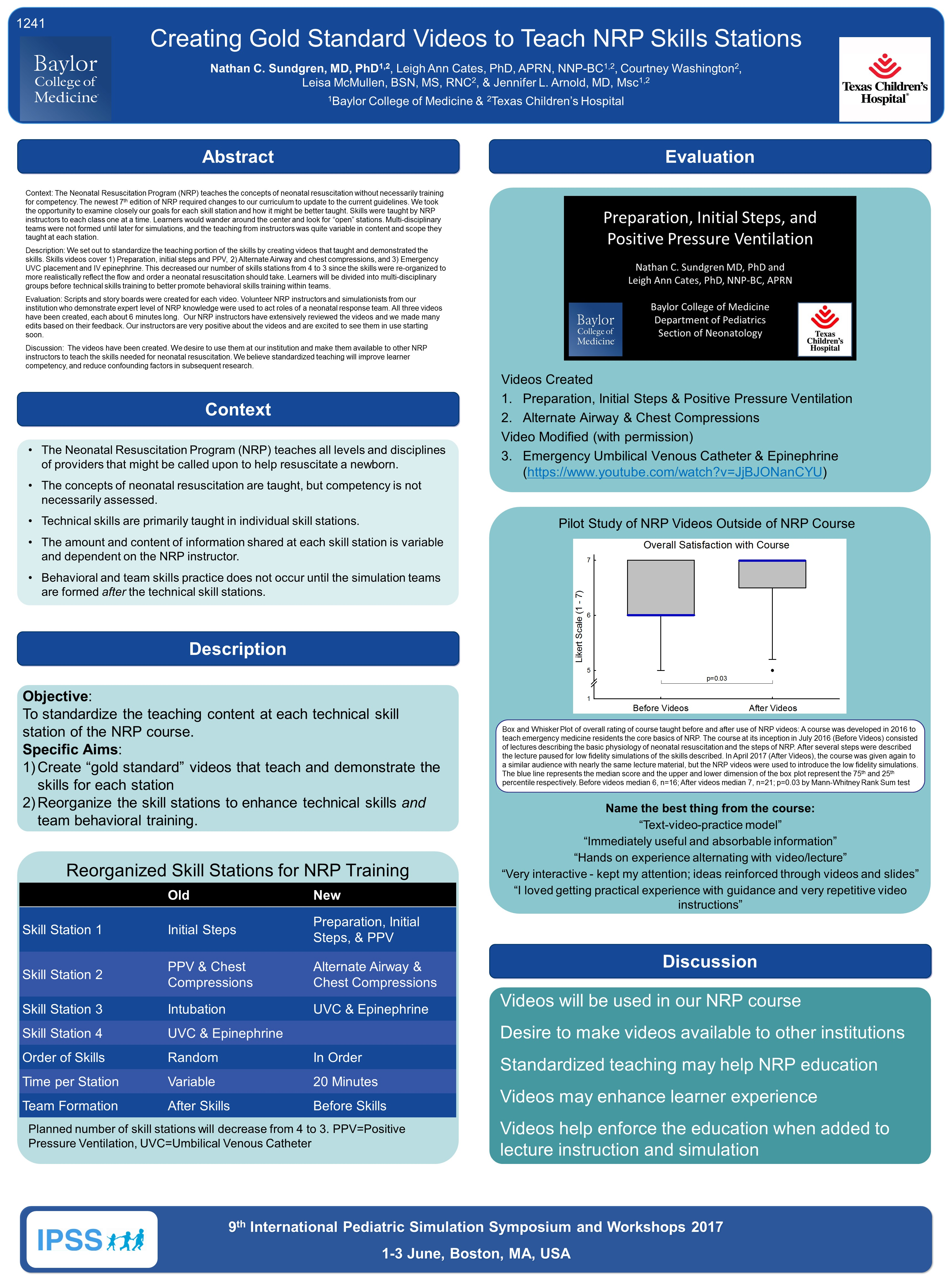
Evaluation: Scripts and story boards were created for each video. Volunteer NRP instructors and simulationists from our institution who demonstrate expert level of NRP knowledge were used to act roles of a neonatal response team. All three videos have been created, each about 6 minutes long. Our NRP instructors have extensively reviewed the videos and we made many edits based on their feedback. Our instructors are very positive about the videos and are excited to see them in use starting soon.
Discussion: The videos have been created. We desire to use them at our institution and make them available to other NRP instructors to teach the skills needed for neonatal resuscitation. We believe standardized teaching will improve learner competency, and reduce confounding factors in subsequent research.