Abstract
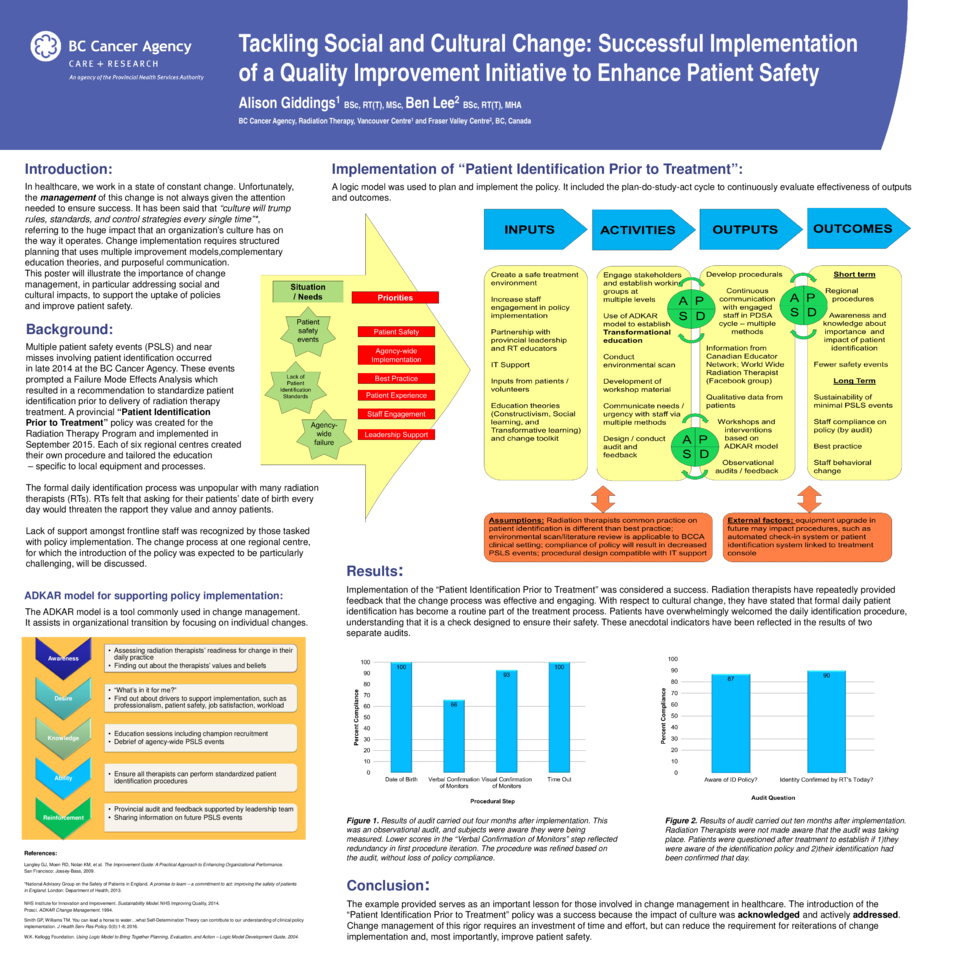
Purpose: This poster describes a quality improvement initiative that occurred in radiation therapy departments across British Columbia. This initiative harnessed the investigational response to several safety events in the province. The reformative change involved the implementation of a Provincial Patient Identification Policy specific to radiation therapy delivery, across multiple centres with different operational needs. The process at one regional centre, for which the change was recognized as particularly unpopular, will be detailed.
Methods: The operationalization of the “Provincial Patient Identification Policy” utilized quality improvement fundamentals from several change models. Some of these activities include: engaging staff at all levels, studying and refining the change with input from stakeholders, and, most importantly, creating autonomous motivation through transformational education. This initiative involved not only a simple procedural change, but also challenged deeply held beliefs and assumptions of Radiation Therapists in British Columbia. Radiation Therapists believed strongly that involving patients in daily identification protocols would create barriers to developing rapport and trust. As such, education involving the patient identification policy had to tackle the social aspects of change implementation, as well as the increasing effort to focus on improving patient experience by health care providers. Early on, this was recognized by Clinical Educators, and actively addressed. Efforts to educate about the change were well coordinated with the implementation of the change itself. After several months, audits were performed to establish compliance.
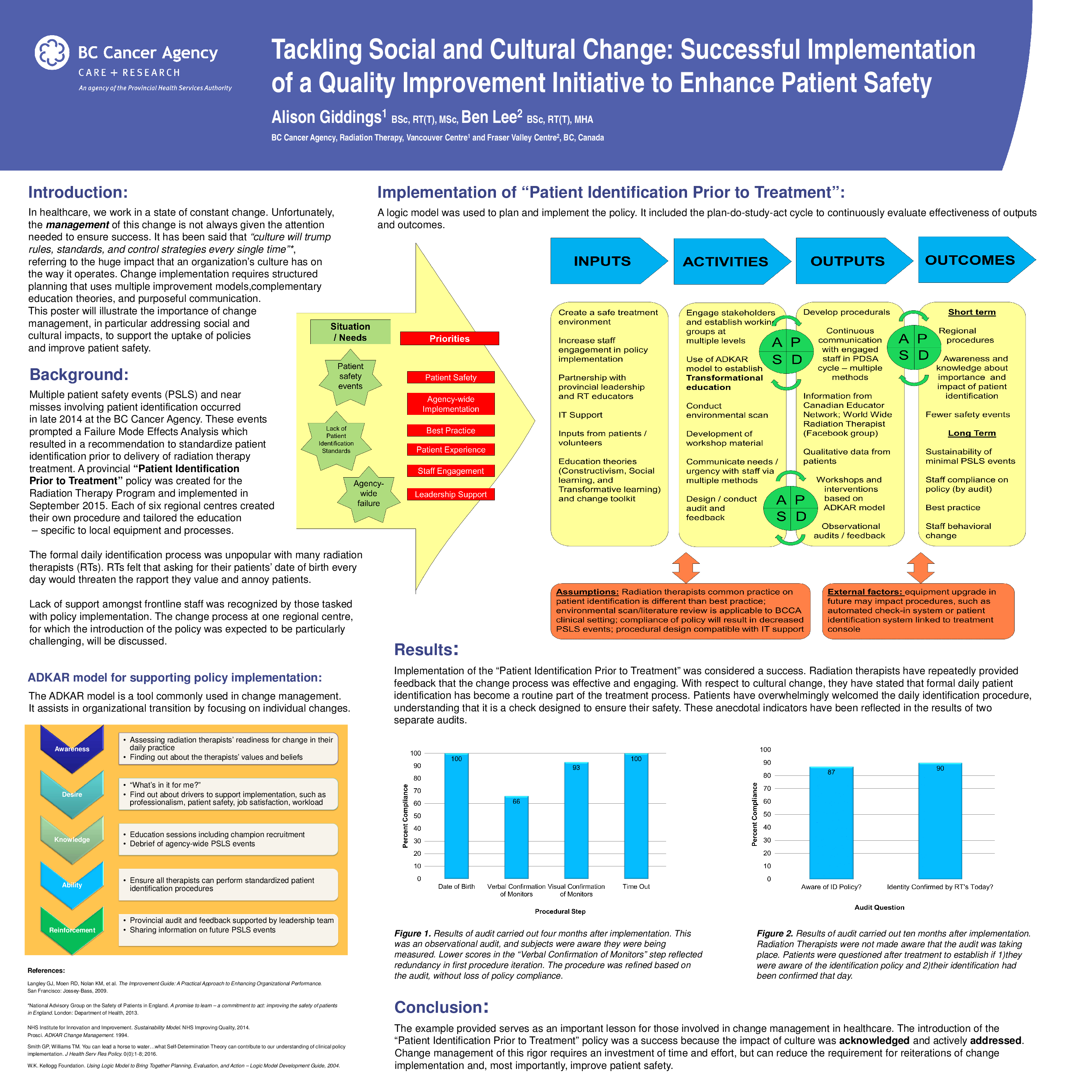
Results: Preliminary audits performed on patient identification indicate that the implementation of the “Provincial Patient Identification Policy” has been a success. Two types of audits were carried out. At four months post implementation, an observational audit was performed. Participants were aware they were being audited. At 10 months post implementation, an audit took place for which participants were unaware that they were being measured.
Conclusion: The example provided serves as an important lesson for those involved in change management in healthcare. The introduction of the “Patient Identification Prior to Treatment” policy was a success because the impact of culture was acknowledged and actively addressed. Change management of this rigor requires an investment of time and effort, but can reduce the requirement for reiterations of change implementation and, most importantly, improve patient safety.