Abstract
Introduction: Over 2 million cases of breast cancer are diagnosed each year making it the most frequently diagnosed malignancy worldwide. As of 2022, breast cancer is the 5th most common cause of death due to cancer globally. Fortunately, mortality rates have dropped in the last decade due to an increase in routine mammogram screenings. Invasive lobular carcinoma (ILC) is the second most common form of breast cancer, after invasive ductal carcinoma, occurring in 10-15% of invasive breast cancers. Prognosis is dependent on tumor stage. If ILC is detected and treated early, prognosis is favorable. Prognostic factors such as hormone receptor positivity and low-grade growth are typical of ILC. ILC is typically treated with surgical excision. Therapy after surgery involves hormonal therapy in conjunction with possible chemotherapy and radiation.
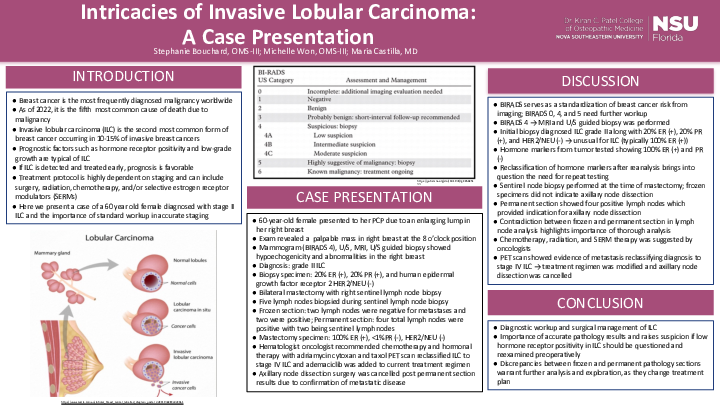
Case Description: We present the case of a 60-year-old female who presented to her primary care physician complaining of a palpable enlarging lump in her right outer breast. She denied any symptoms of breast pain, nipple drainage, nipple inversion or palpation of axillary lymph nodes. Oral contraception was used for a few months at age 24. Patient is G11P6 with first birth at age 24. First menarche was at 12-years-old and last menstrual period was at 46-years-old. Patient has no history of hormone replacement therapy. Patient has no family history of breast cancer. On examination palpable mass in the upper outer right breast at the 8 o’clock position was felt.
After diagnostic imaging and biopsy, grade 2 ILC with 20% ER positivity, 20% PR positivity and human epidermal growth factor receptor 2 (HER2/NEU) negative was determined. The patient was counseled and choose to undergo a bilateral breast mastectomy with right sentinel lymph node biopsy. A sentinel node biopsy was performed on the right in conjunction with right mastectomy. Six total lymph nodes were identified and sent to pathology. Breast pathology indicated invasive carcinoma present at the margin with skeletal muscle invasion. Two right sentinel lymph nodes and two right axillary non-sentinel lymph nodes were positive for metastatic lobular carcinoma. Postoperatively, the surgeon reordered ER, PR, HER2/NEU from the inpatient lab, a different lab than the initial biopsy assessment. Repeat tumor markers demonstrated ER+ (100%), PR- (<1%), HER2/NEU-.
Postoperatively, the patient met with her radiation oncologist to discuss further treatment. At this time, cancer staging was T2N2M0. The patient met criteria to undergo radiation to the right chest wall and regional lymph nodes due to presence of a large tumor of 4.5 cm, presence of multiple positive nodes, and the presence of a positive deep margin. After the initiation of chemotherapy, she underwent a PET scan which showed a 1.3 cm mediastinal node highly suspicious for malignancy and the patient was reclassified to stage IV ILC.
Discussion: This case illustrates the diagnostic workup and surgical management of ILC. It demonstrates the importance of accurate pathology results and raises suspicion if low hormone receptor positivity in ILC should be questioned and reexamined preoperatively.