Abstract
Introduction: Syphilis is a highly infectious sexually transmitted infection (STI) with a multitude of presentations. The disease is known as “the great imitator” as it can present as other chronic dermatoses, often leading to a difficult and delayed diagnosis. A syphilis superinfection with HIV can lead to an even more distorted course of secondary syphilis as a result of a decreased CD4+ T-cell function, further complicating diagnosis and delaying treatment.
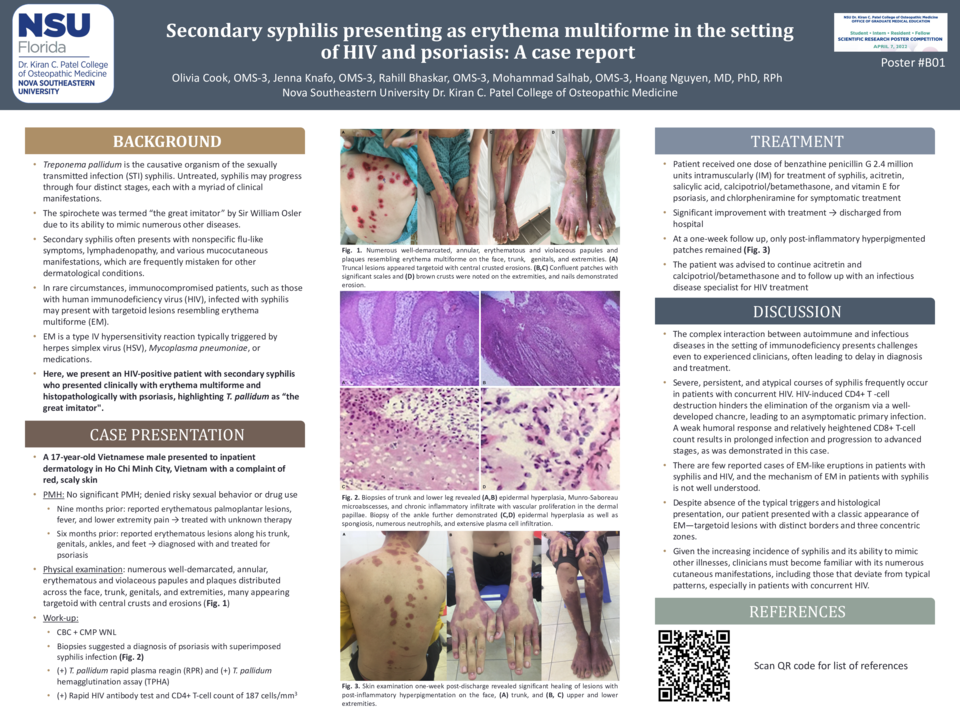
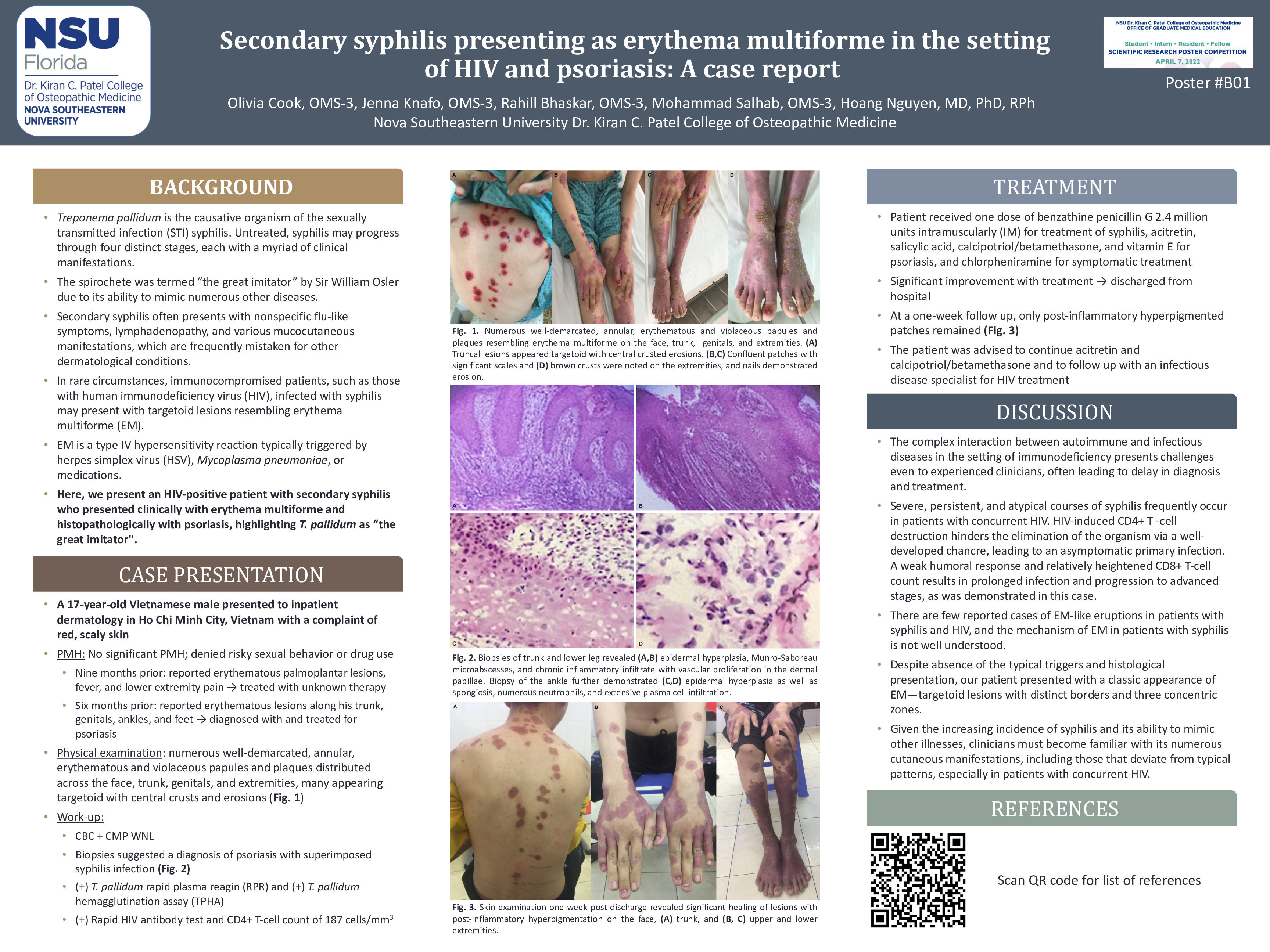
Case Description: We present a case of a 17-year-old Vietnamese male from Dong Nai Province who was initially diagnosed with psoriasis per inpatient dermatology. He presented with a generalized, heterogeneous rash with well-demarcated, annular, erythematous and violaceous papules and plaques distributed across the face, trunk, genitals, and extremities. Many lesions located on the trunk and extremities appeared targetoid, some with central crusted erosions, resembling erythema multiforme. The patient was initially treated with amoxicillin/clavulanic acid, acitretin, vitamin E, chlorpheniramine, zinc, topical salicylic acid, eosin, and calcipotriol/betamethasone for suspected psoriasis. Skin biopsies from the posterior trunk and lower leg revealed epidermal hyperplasia of the stratum spinosum and stratum corneum with the presence of Munro-Saboureau microabscesses. There was also evidence of chronic inflammatory infiltrate with vascular proliferation in the dermal papillae, suggesting psoriasis with an overlying superinfection. A biopsy from the patient’s right ankle also demonstrated spongiosis, numerous neutrophils, and extensive plasma cell infiltration, raising suspicion for syphilis. Further testing confirmed a diagnosis of concurrent secondary syphilis and psoriasis, complicated by undiagnosed HIV. Benzathine penicillin G IM was administered, and acitretin, salicylic acid, calcipotriol/betamethasone, chlorpheniramine, and vitamin E were continued to treat the psoriasis. All other medications were discontinued. The lesions revealed significant improvement and the patient was discharged on day 17 of hospitalization. The patient was advised to continue acitretin and calcipotriol/betamethasone and to follow up with an infectious disease specialist for HIV treatment.
Discussion: This case illustrates serology-confirmed secondary syphilis and pathology-confirmed psoriasis in an HIV-positive patient presenting clinically with erythema multiforme-like lesions. This patient’s unique presentation allowed an opportunity to observe the dermatologic manifestations of numerous maladies at varying degrees in their courses.