Abstract
Presented at: CAEP, Quebec City, CAN; June 4-8, 2016
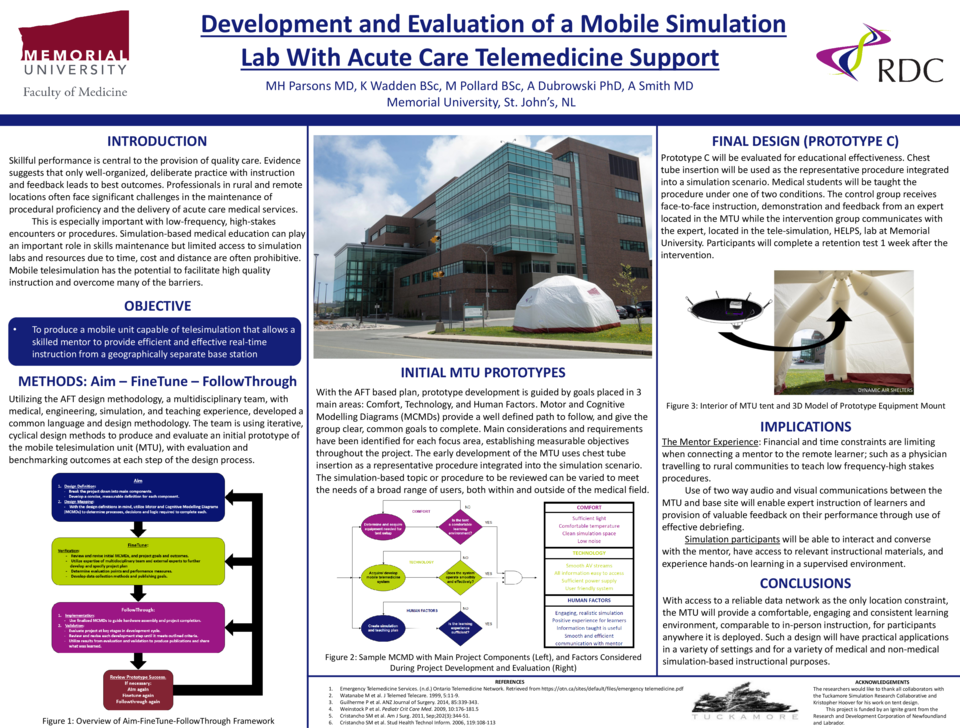
Introduction / Innovation Concept: Skillful performance is central to the provision of quality healthcare. Well-organized, deliberate practice with instruction and feedback leads to the best learning and patient outcomes. Professionals in rural/remote locations often face significant challenges in maintaining procedural proficiency and delivering acute care medical services. This is especially important with low-frequency high-stakes procedures. Simulation can play an important role in skills maintenance but limited access to simulation labs and resources in rural areas due to time, cost and distance are often prohibitive. Mobile telesimulation has the potential to facilitate high-quality instruction and overcome these barriers. Our goal is to develop a mobile simulation unit (MSU) that uses acute-care telemedicine mentoring techniques to meet the needs of rural physicians.
Methods: The MSU design process is a prototype development series with qualitative results from each prototype (A and B) informing design and development of the next. This serves as an assessment of the functionality and set-up of the MSU for housing the simulation equipment/mannequin and providing an acceptable learning environment. The final design (C) will be evaluated for educational effectiveness. Medical students will be taught endotracheal intubation on a mannequin in the MSU under one of 2 conditions. The experimental group will receive instruction, demonstration and feedback from an expert in the telesimulation lab at Memorial University. The control group will receive the same instructions and feedback face-to-face from an expert located in the MSU. Participants will complete a retention test 1 week after the intervention. Performance between the 2 groups will be compared and user satisfaction will be assessed.
Curriculum, Tool, or Material: The MSU will be a portable, inflatable structure equipped with telecommunication equipment to provide efficient interaction between the rural/remote learner and their instructor at a different site. The design and components of the MSU will facilitate easy transport and deployment for telesimulation in rural/remote areas. A combination of fixed and wearable cameras will facilitate instruction, demonstration and feedback to the learner. Conclusion: Mobile telesimulation may play an important role in overcoming the barriers of geography, cost and access to expert instruction. Implications of this research are far reaching and extend beyond healthcare education and training.