Abstract
Presented at: Medical Education Scholarship Forum; St. John's, Newfoundland; December, 2015
Purpose: Simulation-based medical education (SBME), as a teaching, learning and assessment tool, has seen increased application in many areas of medicine. In emergency Medicine (EM), trainees must develop a specific skill set to enable smooth transition to clinical practice and to ensure patient encounters have the best possible outcomes. To guarantee that residents develop the required expertise in core EM topics, procedural skills and crisis resource management it’s important to supplement hands-on clinical learning with interactive simulation-based cases. To maximize the benefits residents receive from the simulation component of their training, we compiled the EM SIM Book including information from key resources and examples relevant to our local setting.
Methods: The EM Simulation document draws from a number of sources, including the course manual Center for Medical Simulation: Institute for Medical Simulation Comprehensive Instructor Workshop, www.harvardmedsim.org. Local resources were also utilized, including Memorial University’s Clinical Learning and Simulation Centre and the Tuckamore Simulation Research Collaborative. Further information, largely surrounding procedural skills, came from the textbook Roberts and Hedges: Clinical Procedures in Emergency Medicine. Permission was obtained from all sources for small-scale distribution and use in academia/teaching.
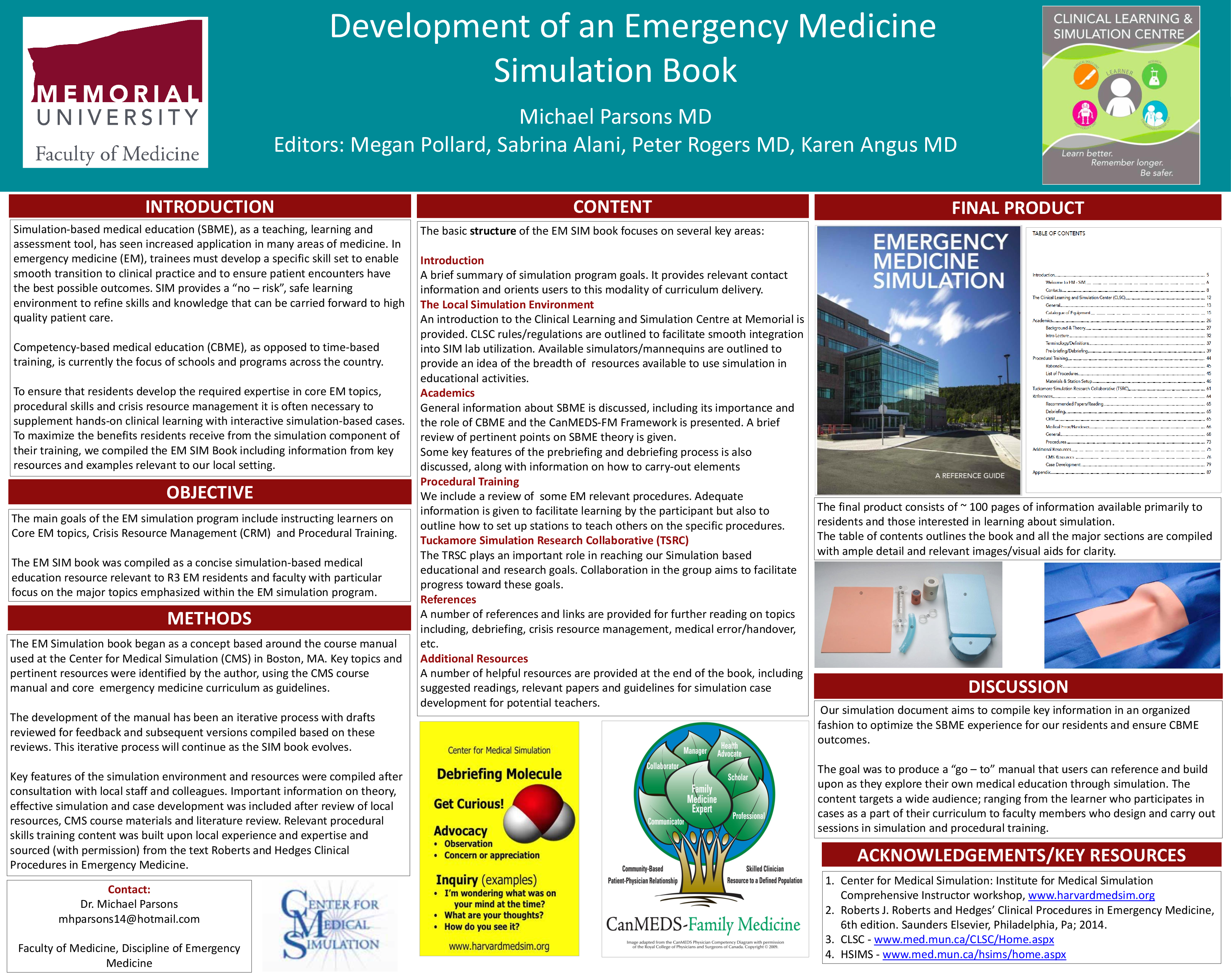
Results: The final product consists of 80+ pages of information introducing residents to local simulation resources/settings, providing relevant background information and orienting residents to this modality of curriculum delivery. Theory and rationale behind simulation use is outlined and information on debriefing is highlighted to show it’s key role in using simulation as an educational tool. Specific information on a number of core EM procedures is also included, outlining necessary materials for each procedure and providing tips on setting up practice stations for these skills. A number of references and links are provided for further reading on topics including, debriefing, crisis resource management, medical error/handover, etc. Further learning resources are noted, including information on case development for potential teachers.
Conclusions: Simulation is a valuable tool for teaching many skills in the field of medicine. This is particularly true for the broad knowledge base and skill-set required in Emergency Medicine. Our simulation document aims to compile key information in an organized fashion to optimize the SBME experience for our residents.